You've been experiencing persistent back pain, and your doctor suggests an X-ray. But can this imaging technique really reveal if you have a herniated disc? This is a common question for many individuals facing back discomfort and seeking answers through medical imaging. Understanding the capabilities and limitations of X-rays is crucial for anyone dealing with back pain or suspected spinal issues.
Understanding the purpose of X-rays in diagnosing back pain
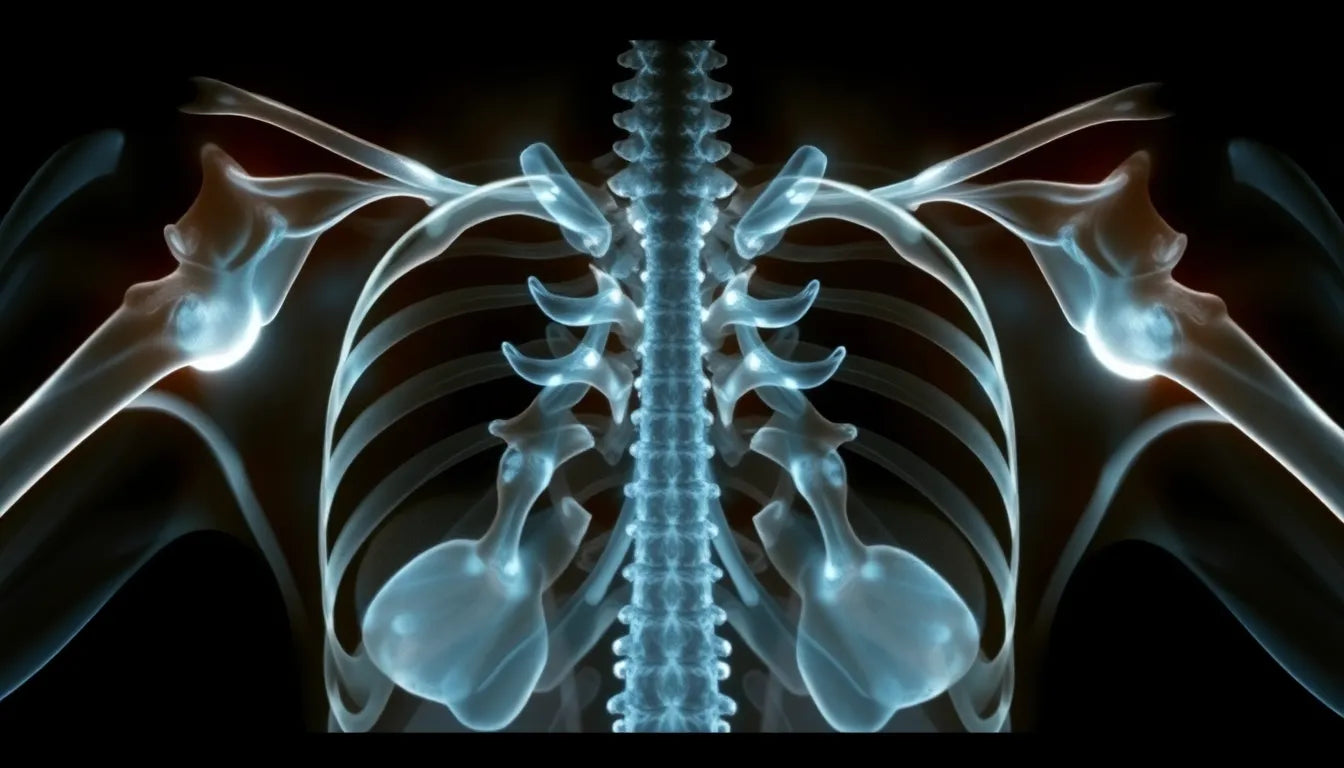
X-rays are a widely used diagnostic tool, particularly valued for their ability to visualize bones. When it comes to diagnosing back pain, X-rays can be instrumental in ruling out certain conditions such as fractures, infections, or tumors. However, when it comes to identifying soft tissue problems, like a herniated disc, X-rays have significant limitations. This post aims to explore these limitations and discuss alternative diagnostic methods that may be necessary for a comprehensive evaluation.
Why knowing the limits of X-rays is important
For those experiencing back pain, understanding what an X-ray can and cannot show is essential. While X-rays are excellent for assessing the alignment of the vertebrae and detecting bone-related issues, they fall short when it comes to revealing the condition of intervertebral discs. Intervertebral discs are composed of soft tissue, which X-rays cannot adequately visualize. As a result, relying solely on X-rays for diagnosing a herniated disc could lead to an incomplete or inaccurate assessment of your spine's health.
This understanding is crucial, as it can guide patients and healthcare providers in selecting the most appropriate diagnostic approach. By recognizing the limitations of X-rays, patients can better advocate for themselves and seek additional tests that provide a clearer picture of their spinal health. This knowledge empowers individuals to make informed decisions about their medical care and pursue the most effective treatment options available.
In the following sections, we will delve deeper into the specific limitations of X-rays in detecting herniated discs and explore alternative diagnostic methods that offer more detailed insights into spinal conditions. This comprehensive approach ensures that individuals receive accurate diagnoses and effective treatment plans tailored to their specific needs.
limitations of x-rays in detecting herniated discs
X-rays have long been a staple in medical diagnostics, particularly for visualizing bone structures. However, their utility in assessing soft tissue conditions, such as herniated discs, is limited. This is primarily because X-rays are designed to capture images of dense structures like bones, while soft tissues, including intervertebral discs, do not absorb X-rays in the same way. As a result, the nuances of soft tissue abnormalities, like a herniated disc, remain invisible on a standard X-ray image.
According to experts at Discseel and Regenerative Spine and Joint, while X-rays can reveal changes in bone structure, such as shifts in vertebrae alignment or disc space height, they cannot directly depict herniated discs. This limitation stems from the inability of X-rays to penetrate and visualize the soft, gel-like material of the intervertebral discs. Therefore, while an X-ray might suggest that a disc problem exists due to changes in the spine's alignment, it cannot confirm the presence of a herniated disc.
alternative diagnostic methods for herniated discs
Given the limitations of X-rays, other imaging techniques are often employed to accurately diagnose herniated discs. Magnetic Resonance Imaging (MRI) is considered the gold standard for this purpose. MRIs use magnetic fields and radio waves to produce detailed images of the body's soft tissues, providing a clear view of the intervertebral discs and surrounding structures. This allows healthcare providers to assess the condition of the discs and any potential nerve involvement.
CT scans and myelograms also play a role in diagnosing spinal conditions. CT scans offer cross-sectional images that can help visualize bone and, to some extent, soft tissue structures. Myelograms involve the injection of a contrast dye into the spinal canal, enhancing X-ray images to better visualize spinal cord and nerve root compressions. These methods, while less commonly used than MRIs, can be valuable in certain diagnostic scenarios.
Electromyograms (EMG) are another tool in the diagnostic arsenal, particularly for evaluating nerve function. By measuring the electrical activity of muscles, EMGs can help pinpoint the location of nerve compression caused by a herniated disc. This information is crucial for determining the appropriate treatment plan.
importance of clinical evaluation
While imaging techniques are invaluable in diagnosing herniated discs, they should be complemented by a thorough clinical evaluation. Physical and neurological exams provide critical context for imaging results. During these exams, healthcare providers assess factors such as muscle strength, reflexes, and sensory function to gain a comprehensive understanding of the patient's condition.
Clinical evaluations, combined with imaging results, allow for a more accurate diagnosis and tailored treatment plan. By integrating patient history, physical examination findings, and imaging data, healthcare providers can develop a holistic understanding of the patient's spinal health, ensuring that treatment addresses the root cause of the pain rather than just the symptoms.
In conclusion, while X-rays are a valuable tool for ruling out certain conditions, they are not sufficient for diagnosing herniated discs. Alternative imaging methods like MRIs, along with comprehensive clinical evaluations, are essential for an accurate diagnosis. Understanding the limitations of X-rays empowers patients to seek the most appropriate diagnostic and treatment options, ultimately leading to better outcomes and improved spinal health.
Integrating diagnostic approaches for accurate results
When it comes to diagnosing herniated discs, a comprehensive approach is paramount. Relying solely on X-rays can lead to incomplete assessments, as they primarily capture bone structures and are not equipped to visualize soft tissues like intervertebral discs. For a precise diagnosis, combining various diagnostic methods is essential. This includes imaging techniques such as MRI and CT scans, alongside clinical evaluations that consider a patient's medical history and physical examination results.
For instance, a patient experiencing back pain may initially undergo an X-ray to rule out bone-related issues. If the results indicate potential disc problems, an MRI might follow to provide a detailed view of the soft tissues, confirming the presence of a herniated disc. Meanwhile, physical and neurological exams help assess the impact on nerve function, guiding the treatment plan.
Case studies: real-world application
Consider the case of a patient, John, who experienced chronic lower back pain. Initial X-rays showed no bone abnormalities, prompting his healthcare provider to order an MRI. The MRI revealed a herniated disc compressing a nerve root, explaining John's symptoms. With this comprehensive diagnosis, John underwent a tailored treatment plan, including physical therapy and lifestyle modifications, which significantly improved his condition.
In another example, Sarah, a patient with similar symptoms, had an X-ray that suggested disc space narrowing. An MRI confirmed a herniated disc, and an electromyogram (EMG) further pinpointed the affected nerve. This multi-faceted diagnostic approach allowed Sarah's healthcare team to develop an effective intervention strategy, combining medication and targeted exercises to alleviate her pain.
Frequently Asked Questions
Can an X-ray detect a herniated disc?
No, X-rays cannot directly show a herniated disc. They are primarily used to rule out other conditions affecting the bones.
Why is an MRI preferred over an X-ray for diagnosing a herniated disc?
MRIs provide detailed images of soft tissues, including discs and nerves, making them more effective for diagnosing herniated discs.
What should I expect during an MRI scan?
An MRI is a non-invasive procedure that uses magnetic fields to create detailed images. You will lie still inside a machine, and the process typically takes 30-60 minutes.
Can a herniated disc heal on its own?
In some cases, herniated discs can improve over time with rest, physical therapy, and proper care. However, severe cases may require medical intervention.
In conclusion, understanding the limitations of X-rays in diagnosing herniated discs is crucial for effective medical care. By integrating advanced imaging techniques and thorough clinical evaluations, healthcare providers can ensure accurate diagnoses and tailored treatment plans. This holistic approach not only addresses the root cause of back pain but also enhances patient outcomes, leading to improved spinal health and quality of life.