When faced with the discomfort and disruption caused by a herniated disc in the neck, many individuals find themselves at a crossroads. The decision of whether to undergo surgery or explore non-surgical treatments is a significant one, influencing not only physical health but overall quality of life. Understanding the nature of a herniated disc and the symptoms it presents is the first step toward making an informed choice.
understanding herniated discs in the neck
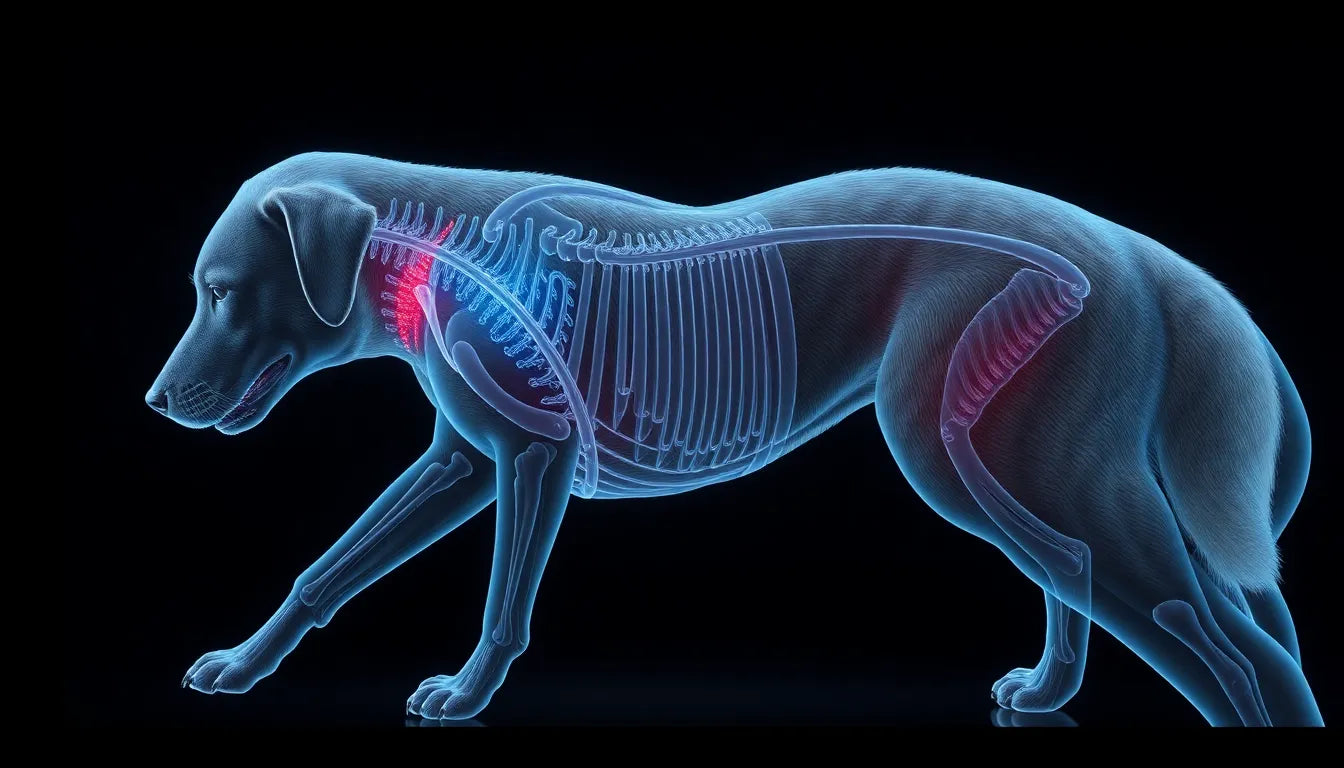
A herniated disc, often referred to as a slipped or ruptured disc, occurs when the inner gel-like core of a spinal disc pushes through its outer layer. This condition is particularly common in the cervical spine—the neck region—due to the mobility and stress this area endures. Many individuals experience this issue, and it can manifest through symptoms such as persistent neck pain, radiating arm pain, numbness, and even weakness in the affected areas. These symptoms can significantly impact daily activities, making it crucial to address the problem effectively.
the decision dilemma: surgery or not?
The central question for those suffering from a herniated disc in the neck is whether to opt for surgical intervention or to pursue non-surgical treatments. This decision is not one to be taken lightly, as it carries implications for long-term health and well-being. Surgery might offer a quicker resolution to severe symptoms, but it also involves risks and a recovery period. On the other hand, non-surgical options may require more patience and commitment but often present fewer risks.
importance of informed decision-making
Making an informed decision regarding treatment is essential, as the right choice can dramatically enhance a patient's quality of life. A successful treatment plan can alleviate pain, restore function, and enable individuals to return to their normal activities. However, it's important to balance the potential benefits of surgery against its risks, considering factors such as the severity of symptoms, overall health, and lifestyle impacts. Non-surgical treatments, like physical therapy and medication, can also offer relief and should be considered as part of the decision-making process.
Ultimately, the path to addressing a herniated disc in the neck is a personal one, requiring a thorough understanding of the condition, available treatments, and individual health needs. Whether choosing surgery or not, the goal remains the same: to improve health outcomes and enhance quality of life through informed, thoughtful decisions.
surgical options and diagnosis for herniated discs in the neck
When considering treatment for a herniated disc in the neck, the first step often involves a thorough diagnosis. Advanced imaging techniques such as MRI or CT scans with myelography are typically employed to confirm the presence and extent of the herniated disc. These diagnostic tools provide detailed images of the cervical spine, allowing healthcare professionals to assess the severity and exact location of the herniation.
Once a diagnosis is confirmed, several surgical options may be considered, each tailored to the specific needs of the patient. One of the most common procedures is the anterior cervical discectomy and fusion (ACDF). This surgery involves removing the herniated disc and fusing the adjacent vertebrae to stabilize the spine. ACDF is often recommended for patients experiencing severe symptoms that do not respond to conservative treatments. While it is effective in relieving pain, it may limit neck mobility.
Another surgical option is artificial cervical disc replacement, which aims to preserve neck mobility by replacing the damaged disc with an artificial one. This procedure is suitable for patients who wish to maintain a greater range of motion post-surgery. However, it may not be appropriate for everyone, especially those with advanced degenerative disc disease.
Posterior cervical decompression (microdiscectomy) is a less invasive procedure that involves removing the portion of the disc that is pressing on the nerve. This approach is typically recommended for patients with specific nerve compression symptoms. Recovery from this surgery is often quicker, but the procedure may not be suitable for all types of herniations.
Success rates for these surgical procedures are generally high, ranging from 80-90%. However, like any surgery, they come with potential risks, including infection, nerve damage, or issues related to the fusion or artificial disc.
conservative treatment approaches for herniated discs in the neck
Before opting for surgery, many patients explore conservative treatment options. These non-surgical approaches can effectively manage symptoms and improve quality of life for those with less severe conditions. Medication is often the first line of treatment, with non-steroidal anti-inflammatory drugs (NSAIDs) being commonly prescribed to reduce pain and inflammation.
Physical therapy plays a crucial role in conservative management. Tailored exercises and stretches can help alleviate pain, improve neck mobility, and strengthen the muscles supporting the cervical spine. A physical therapist can also provide guidance on proper posture and ergonomic adjustments to prevent further strain on the neck.
Epidural steroid injections are another option for patients experiencing significant pain. These injections deliver anti-inflammatory medication directly to the affected area, providing relief from pain and swelling. While effective for many, this treatment is typically used in conjunction with other therapies and not as a standalone solution.
Lastly, rest and lifestyle modifications are essential components of conservative treatment. Using ergonomic aids, such as supportive pillows and adjustable chairs, can help reduce strain on the neck. Additionally, lifestyle changes like regular exercise, maintaining a healthy weight, and avoiding activities that exacerbate symptoms can significantly impact recovery and symptom management.
when surgery is recommended for herniated discs in the neck
Surgery is typically considered when conservative treatments fail to provide relief or when symptoms worsen. Persistent arm pain or weakness, signs of myelopathy (spinal cord compression), and lack of improvement with non-surgical approaches are common indicators for surgical intervention. It is crucial to match these symptoms with imaging results to ensure surgery is necessary and likely to be beneficial.
Ultimately, the decision to undergo surgery should be made in consultation with a healthcare professional, considering the individual's overall health, lifestyle, and personal preferences. By understanding the available treatment options and their implications, patients can make informed decisions that align with their goals for recovery and quality of life.
Comparative analysis of surgical options for herniated discs in the neck
Deciding on the appropriate surgical intervention for a herniated disc in the neck involves weighing the pros and cons of each procedure. Below is a comparative table highlighting the key features of the three primary surgical options: ACDF, artificial cervical disc replacement, and posterior cervical decompression (microdiscectomy).
| Surgical Option | Pros | Cons |
|---|---|---|
| Anterior Cervical Discectomy and Fusion (ACDF) | High success rate, effective pain relief, stabilizes the spine | May limit neck mobility, involves fusion of vertebrae |
| Artificial Cervical Disc Replacement | Preserves neck mobility, suitable for maintaining range of motion | Not suitable for advanced degenerative disc disease, potential for disc wear |
| Posterior Cervical Decompression (Microdiscectomy) | Less invasive, quicker recovery, effective for nerve compression | Not suitable for all herniations, may not address all symptoms |
Patient experiences and testimonials
Understanding patient experiences can provide valuable insights into the decision-making process for herniated disc surgery. For instance, Jane, a 45-year-old office worker, shared her journey through conservative treatments before opting for ACDF. "I tried physical therapy and medication for months," she explained, "but the persistent arm pain and numbness affected my work and quality of life. After the surgery, I noticed significant improvement, and within a few months, I was back to my normal activities."
Similarly, Tom, a 50-year-old avid cyclist, chose artificial cervical disc replacement to maintain his active lifestyle. "Preserving my neck mobility was crucial for me," Tom noted. "The procedure allowed me to continue cycling without the constant worry of limited movement."
Recovery and post-surgery care
Recovery from herniated disc surgery varies depending on the type of procedure performed. Typically, patients undergoing ACDF may expect a recovery period of six to twelve weeks, during which neck braces might be used to support the healing process. In contrast, those who opt for artificial disc replacement or microdiscectomy often experience a quicker recovery, with many returning to normal activities within a few weeks.
Post-surgery care is critical to ensure successful outcomes. Patients are advised to follow their healthcare provider's guidelines, including attending follow-up appointments, engaging in prescribed physical therapy, and avoiding strenuous activities that may strain the neck. Proper post-operative care helps in managing potential complications and supports a smoother recovery.
Frequently asked questions
What are the symptoms of a herniated disc in the neck?
Common symptoms include persistent neck pain, arm pain, numbness, tingling, and weakness in the shoulder, arm, or hand. These symptoms can vary in intensity and may affect daily activities.
How long does it take to recover from neck surgery for a herniated disc?
Recovery time varies by procedure. ACDF typically requires six to twelve weeks, while artificial disc replacement and microdiscectomy may allow for a quicker return to normal activities, often within a few weeks.
Are there effective non-surgical treatments for herniated discs?
Yes, non-surgical treatments such as medication, physical therapy, epidural steroid injections, and lifestyle modifications can be effective in managing symptoms for many patients, especially those with less severe conditions.
What are the risks associated with neck surgery for a herniated disc?
Potential risks include infection, nerve damage, issues related to spinal fusion or artificial discs, and the possibility of not achieving the desired pain relief. Discussing these risks with a healthcare professional is crucial before proceeding with surgery.
How can ergonomic aids help in managing or preventing herniated disc symptoms?
Ergonomic aids such as supportive chairs, adjustable desks, and proper posture techniques can help reduce strain on the neck, potentially alleviating symptoms and preventing further injury. These aids are especially beneficial for individuals who spend long hours sitting or working at a computer.