Magnetic Resonance Imaging, or MRI, has revolutionized the way medical professionals diagnose and understand spinal issues. Utilizing powerful magnets and radio waves, MRI technology produces detailed images of the body's internal structures, particularly soft tissues like muscles, ligaments, and discs. This makes it an invaluable tool in diagnosing conditions such as herniated discs, which can significantly impact spinal health and nerve function.
A herniated disc occurs when the soft inner gel of a spinal disc, known as the nucleus pulposus, pushes through a tear in the tougher outer layer called the annulus fibrosus. This protrusion can press against nearby nerves, leading to symptoms such as pain, numbness, or weakness in the limbs. Identifying herniated discs accurately on MRI scans is crucial for effective treatment planning, allowing healthcare providers to tailor interventions that address the root cause of a patient's discomfort.
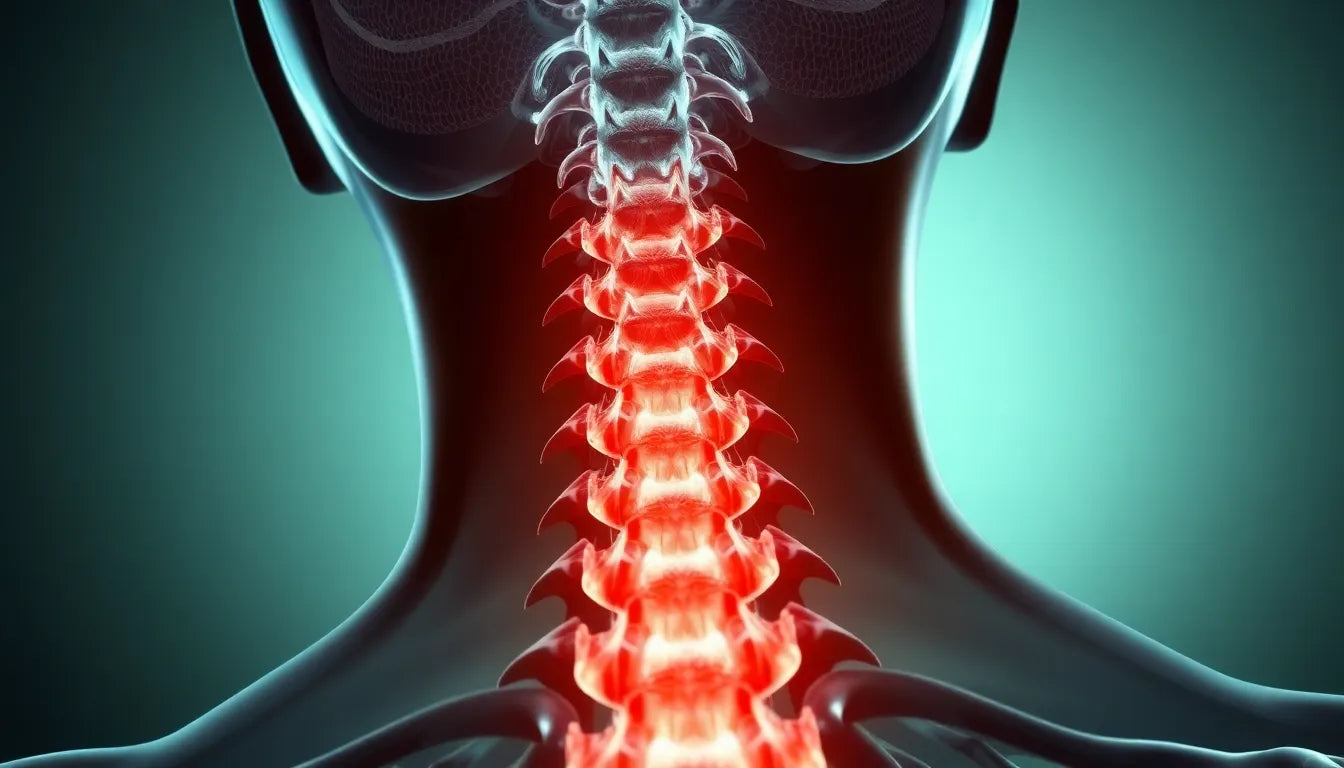
the significance of MRI in diagnosing herniated discs
MRI is the preferred imaging method for evaluating soft tissues, including spinal discs and nerves, due to its ability to produce high-resolution images without exposing patients to radiation. This is particularly important in diagnosing herniated discs, as it allows for a clear visualization of the disc material and its relationship with surrounding structures. On an MRI scan, a herniated disc typically appears as a bulging or protruding area that may compress adjacent nerve roots or the spinal cord.
In this blog post, we will delve into the visual characteristics of herniated discs on MRI scans and explore the clinical implications of these findings. Readers will learn how to identify herniated discs on MRI images and understand the significance of these observations in the context of spinal health. By enhancing your understanding of MRI technology and its application in diagnosing herniated discs, you can better appreciate the role of this advanced imaging technique in guiding treatment decisions and improving patient outcomes.
visual characteristics of a herniated disc on MRI
When examining an MRI scan, a herniated disc is primarily identified by the protrusion of disc material beyond its usual boundaries. This protrusion is often the nucleus pulposus pushing through the annulus fibrosus. On T2-weighted images, which are commonly used for spinal assessments, healthy discs typically appear bright due to their high water content. In contrast, a herniated disc may present as a darker, bulging area that disrupts the normal contour of the disc, often pressing into the spinal canal or nerve space.
Radiologists frequently use annotated images to mark herniated discs and any associated nerve compression. These annotations, often with arrows, help highlight the displaced disc material and its impact on nearby nerves. This visual aid is crucial for both diagnosis and for explaining the condition to patients, ensuring clear communication about the nature of the herniation and its potential effects.
key features to identify on MRI scans
nerve compression
One of the critical indicators of a herniated disc on an MRI is evidence of nerve compression. This can be seen as the pinching or displacement of nerve canals by the protruding disc material. Identifying this compression is essential, as it directly correlates with the patient's symptoms, such as pain or numbness in the affected areas.
disc protrusion and annular tear
An MRI can reveal the specific location where the outer layer of the disc, the annulus fibrosus, has ruptured, allowing the inner gel-like material to protrude. This manifests as a spot of contrasting density on the scan, indicating a change in the disc's structure. Recognizing these changes is vital for diagnosing the severity of the herniation and planning appropriate treatment.
disc migration
In some cases, the herniated disc material can migrate from its original position, either upwards or downwards along the spinal column. This migration can alter the site of nerve compression, which might affect the symptoms experienced by the patient. On an MRI, this is visualized as a mass of similar intensity to the disc but displaced from the usual disc space, providing a clear indication of the herniation's dynamic nature.
signal intensity and age of herniation
The signal intensity of a herniated disc on MRI can provide insights into the age of the herniation. Fresh herniations often appear brighter on T2-weighted images due to the presence of more water content, while older herniations may appear darker as the water content decreases over time. Understanding these variations can help clinicians assess the chronicity of the condition and tailor treatment strategies accordingly.
By comprehending these visual cues and features on MRI scans, healthcare providers can make informed decisions about the best course of action for managing herniated discs. This knowledge not only aids in accurate diagnosis but also enhances the ability to predict potential complications and outcomes, ultimately leading to improved patient care.
Comparative analysis: normal vs. herniated disc
A clear understanding of the differences between a normal and a herniated disc on MRI scans is essential for accurate diagnosis and treatment planning. In a healthy spine, discs appear uniformly bright and are well-contained between the vertebrae. This brightness is due to their high water content, which is easily captured in T2-weighted images. In contrast, a herniated disc disrupts this uniform appearance. It typically presents as a bulging, darker area where the disc material has protruded beyond its normal boundaries. This protrusion can compress nearby nerves, leading to symptoms such as pain or numbness.
Comparative visual aids, such as side-by-side images or diagrams, can effectively highlight these differences. Such visuals are invaluable for both clinicians and patients, as they provide a clear representation of the structural changes that occur in herniated discs. Understanding these visual distinctions helps in correlating MRI findings with clinical symptoms, ensuring that the diagnosis is both accurate and comprehensive.
Clinical implications of MRI findings
The insights gained from MRI scans are crucial in guiding the treatment of herniated discs. MRI results not only confirm the presence of a herniation but also provide detailed information about its size, location, and impact on surrounding structures. This information is vital for developing a tailored treatment plan that addresses the specific needs of the patient.
Correlating MRI findings with patient symptoms is a critical step in the diagnostic process. While some herniated discs may be visible on MRI, not all cause symptoms. Therefore, a comprehensive clinical evaluation, including a detailed patient history and physical examination, is necessary to determine the significance of the MRI findings. This holistic approach ensures that treatment decisions are based on a thorough understanding of the patient's condition, leading to more effective management strategies.
Frequently Asked Questions
What is the role of MRI in diagnosing a herniated disc?
MRI plays a pivotal role in diagnosing herniated discs due to its superior ability to visualize soft tissues, including discs and nerves. Unlike X-rays, which primarily show bones, MRI provides detailed images of the spinal cord, nerve roots, and disc material, making it the preferred imaging method for identifying herniated discs.
How does a herniated disc cause symptoms?
A herniated disc can cause symptoms by compressing nearby nerves. This compression can lead to pain, numbness, or weakness in the areas of the body served by the affected nerves. The severity of symptoms often correlates with the degree of nerve compression seen on MRI.
Can all herniated discs be seen on an MRI?
While MRI is highly effective in detecting herniated discs, several factors can influence their visibility. The size and location of the herniation, as well as the quality of the MRI images, can affect detection. Additionally, some herniations may not cause symptoms, which highlights the importance of correlating MRI findings with clinical evaluations.
What are the treatment options for a herniated disc identified on MRI?
Treatment options for a herniated disc vary based on the severity of the condition and the symptoms experienced by the patient. Conservative treatments include physical therapy, medication, and lifestyle modifications. In cases where conservative measures are ineffective, surgical interventions may be considered to relieve nerve compression and improve symptoms.
Are there any risks associated with MRI scans?
MRI scans are generally considered safe and do not use radiation, unlike other imaging techniques such as X-rays and CT scans. However, patients with certain implants, such as pacemakers, may not be suitable for MRI due to the strong magnetic fields used. It is important to inform the healthcare provider of any implants or medical devices before an MRI scan.