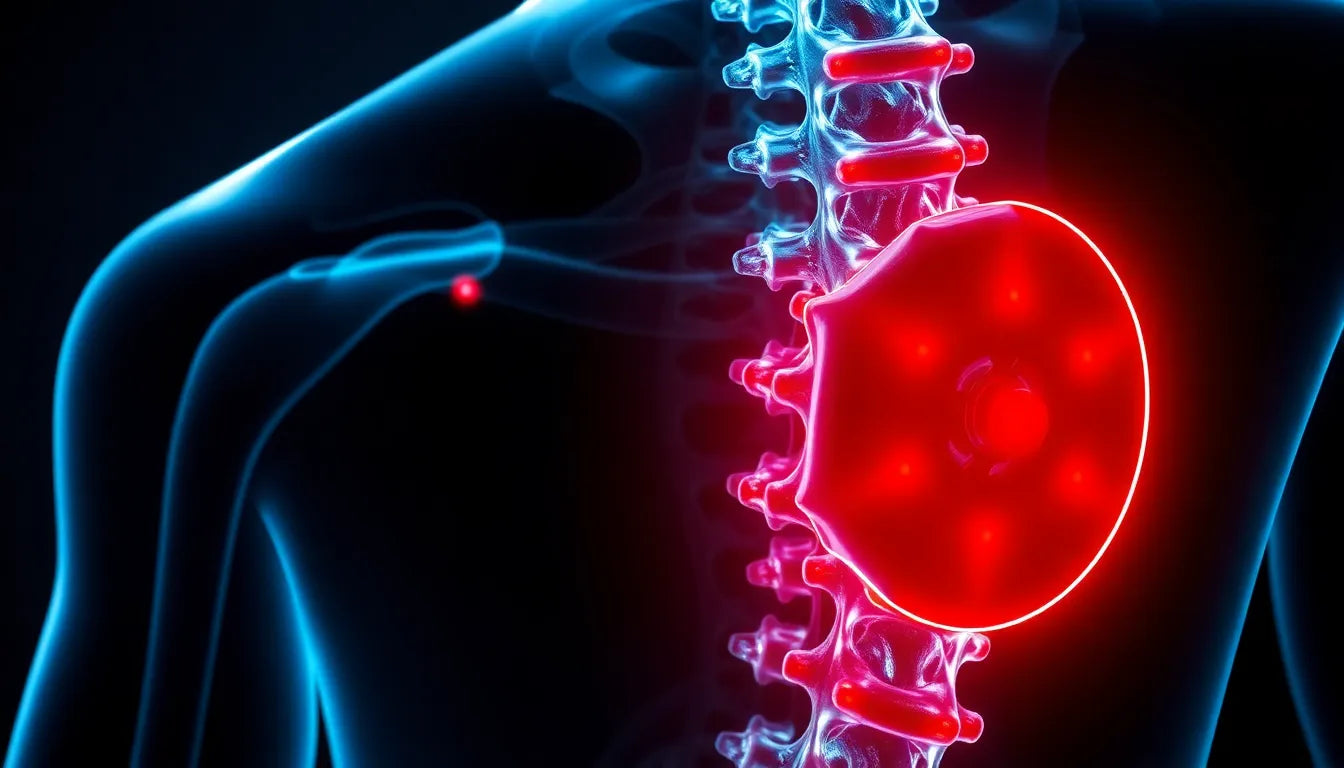
Herniated discs are a common ailment that can significantly disrupt daily life and productivity. Also known as slipped or ruptured discs, these conditions occur when the soft inner gel of a spinal disc protrudes through its tougher outer layer. This can lead to discomfort, pain, and even numbness or weakness in the limbs, depending on the location of the herniation. As such, understanding how to get rid of herniated disc discomfort is crucial for those affected.
Understanding herniated discs
A herniated disc typically arises from wear and tear, also known as disc degeneration. With age, spinal discs lose some of their water content, making them less flexible and more prone to tearing or rupturing with even minor strain or twist. Common causes include improper lifting techniques, sudden heavy strain, or even a traumatic injury. Symptoms often include sharp pain in the back or neck, radiating pain down the arms or legs, and in severe cases, tingling or numbness in the extremities.
Addressing a herniated disc promptly is essential to prevent further complications such as chronic pain or permanent nerve damage. Early intervention can alleviate symptoms and improve quality of life, underscoring the importance of understanding effective treatment options.
Objective of this blog post
The purpose of this blog post is to explore various effective strategies to alleviate herniated disc pain, with a focus on non-surgical and conservative treatments. These methods not only provide relief from pain but also aim to improve spinal health and prevent future occurrences. From physical therapy and lifestyle changes to alternative therapies like yoga and acupuncture, there are numerous ways to address this condition without resorting to surgery. By exploring these options, individuals can make informed decisions about their treatment and work towards a pain-free life.
Non-surgical treatments for herniated disc relief
When it comes to addressing herniated disc pain, non-surgical treatments are often the first line of defense. These approaches focus on relieving pain, reducing inflammation, and promoting healing without the need for invasive procedures.
Physical therapy: strengthening and alignment
Physical therapy plays a pivotal role in managing herniated disc pain. A well-structured physical therapy program can help strengthen core and back muscles, enhance flexibility, and promote proper spinal alignment. Specific exercises, such as pelvic tilts, prone extensions, and gentle stretching, are designed to stabilize the spine and reduce pressure on the affected disc.
Working with a professional physical therapist is crucial as they can tailor a treatment plan to your specific needs. They can guide you through exercises that not only target pain relief but also improve overall spinal health. Regular sessions can lead to significant improvements in mobility and pain levels.
Heat and cold therapy: inflammation and pain management
Alternating between hot and cold therapy can be highly effective in reducing inflammation and alleviating pain associated with a herniated disc. Heat therapy helps to relax tight muscles and improve blood flow, which can promote healing. On the other hand, cold therapy reduces swelling and numbs sharp pain.
To apply heat therapy, use a warm towel or heating pad for about 15-20 minutes. For cold therapy, a cold pack or ice wrapped in a cloth can be applied for the same duration. It's important to alternate between the two, ensuring that the skin is not exposed to extreme temperatures for prolonged periods.
Spinal manipulation: chiropractic care
Spinal manipulation, commonly performed by chiropractors, is another non-surgical approach to managing herniated disc pain. This technique involves applying controlled force to specific joints in the spine to improve alignment and relieve pressure on the herniated disc and surrounding nerves.
Chiropractic care can lead to significant pain relief and improved spinal function. However, it is essential to consult with a qualified chiropractor who can assess your condition and determine the most appropriate treatment plan for you.
Conservative treatments for herniated disc management
Rest and activity modification
Balancing rest and activity is crucial when managing a herniated disc. While it's important to avoid activities that exacerbate pain, complete bed rest is not recommended as it can lead to muscle weakness and stiffness. Instead, focus on modifying daily activities to reduce strain on the back.
Simple changes, such as using ergonomic chairs, avoiding heavy lifting, and incorporating gentle movements, can make a significant difference in managing symptoms. Gradually increasing activity levels as pain subsides can also aid in recovery.
Pain medication and injections
Over-the-counter pain medications, such as ibuprofen or acetaminophen, can be effective in managing mild to moderate pain. For more severe cases, a healthcare provider may recommend epidural steroid injections. These injections deliver anti-inflammatory medication directly to the affected area, reducing inflammation and providing significant pain relief.
It's important to use medications and injections as part of a comprehensive treatment plan and under the guidance of a healthcare professional to avoid potential side effects.
Exploring alternative therapies
Yoga and Pilates: flexibility and strength
Yoga and Pilates are excellent for improving flexibility, strength, and overall spinal health. Gentle poses and exercises, such as the cat-cow stretch, child's pose, and pelvic tilts, are particularly beneficial for individuals with herniated discs.
These practices focus on controlled movements and breathing techniques, which can help alleviate tension and improve posture. Incorporating yoga and Pilates into your routine can complement other treatments and enhance overall well-being.
Acupuncture: pain relief and healing
Acupuncture, an ancient Chinese therapy, involves inserting thin needles into specific points on the body to promote healing and relieve pain. Some studies suggest that acupuncture can be effective in managing herniated disc pain by stimulating the body's natural pain-relieving mechanisms.
While results can vary, many individuals report significant improvements in pain levels and overall comfort. Consulting with a licensed acupuncturist can help determine if this therapy is suitable for you.
Surgical options for herniated disc pain relief
While non-surgical and conservative treatments are effective for many, there are cases where surgical intervention becomes necessary. Surgery is typically considered when a herniated disc causes severe pain that does not improve with other treatments, or when there is significant nerve compression leading to weakness or loss of function.
When surgery is necessary
Surgical options are usually a last resort, reserved for situations where symptoms are debilitating or when there's a risk of permanent nerve damage. Common surgical procedures include microdiscectomy and lumbar laminectomy. A microdiscectomy involves removing the herniated portion of the disc to relieve pressure on the nerve root, while a lumbar laminectomy removes part of the vertebra to widen the spinal canal and alleviate nerve pressure.
These procedures aim to provide immediate pain relief and improve mobility. Recovery times can vary, but many patients experience significant improvement within weeks. Consulting with a spine specialist is crucial to determine the most appropriate surgical approach based on individual circumstances.
Preventive measures to avoid future herniated discs
Preventing herniated discs involves adopting lifestyle changes that promote spinal health. Maintaining a healthy weight is essential, as excess body weight can increase strain on the spine. Regular exercise, focusing on strengthening core muscles, enhances spinal support and flexibility.
Practicing good posture is also vital. Ensure that your workstation is ergonomically designed, and avoid slouching whether sitting or standing. Proper lifting techniques, such as bending at the knees and keeping the back straight, can prevent undue stress on the spine.
Incorporating these changes into daily life can significantly reduce the risk of herniated discs and improve overall spinal health.
Comparative analysis of treatments
Understanding the differences between treatment options can help individuals make informed decisions. Below is a comparative analysis of various treatments for herniated discs:
| Treatment | Effectiveness | Risks | Recovery Time |
|---|---|---|---|
| Physical Therapy | High | Low | Varies, ongoing |
| Heat and Cold Therapy | Moderate | Low | Immediate relief |
| Spinal Manipulation | Moderate | Low to Moderate | Varies |
| Surgery | High | Moderate to High | Weeks to months |
Frequently Asked Questions
What is the fastest way to heal a herniated disc?
Healing a herniated disc quickly involves a combination of rest, physical therapy, and possibly medication to manage pain and inflammation. It's important to follow a comprehensive treatment plan tailored to your specific needs, as advised by a healthcare professional.
Can a herniated disc heal on its own?
In many cases, a herniated disc can heal over time as the body reabsorbs the protruding material. This process can take weeks to months, and factors such as age, overall health, and activity level can influence recovery.
Is walking good for a herniated disc?
Yes, walking is a low-impact activity that can be beneficial for those with a herniated disc. It helps maintain mobility and promotes circulation, which can aid in the healing process. However, it's important to avoid overexertion and consult with a healthcare provider for personalized advice.
How can I prevent a herniated disc from recurring?
Preventive strategies include maintaining a healthy weight, engaging in regular exercise that strengthens the core, practicing good posture, and using proper lifting techniques. Ergonomic adjustments in daily activities can also help reduce strain on the spine.
When should I see a doctor for a herniated disc?
Seek medical attention if you experience severe pain that does not improve with rest, numbness or tingling in the limbs, or weakness that affects daily activities. These symptoms may indicate significant nerve compression requiring professional evaluation.