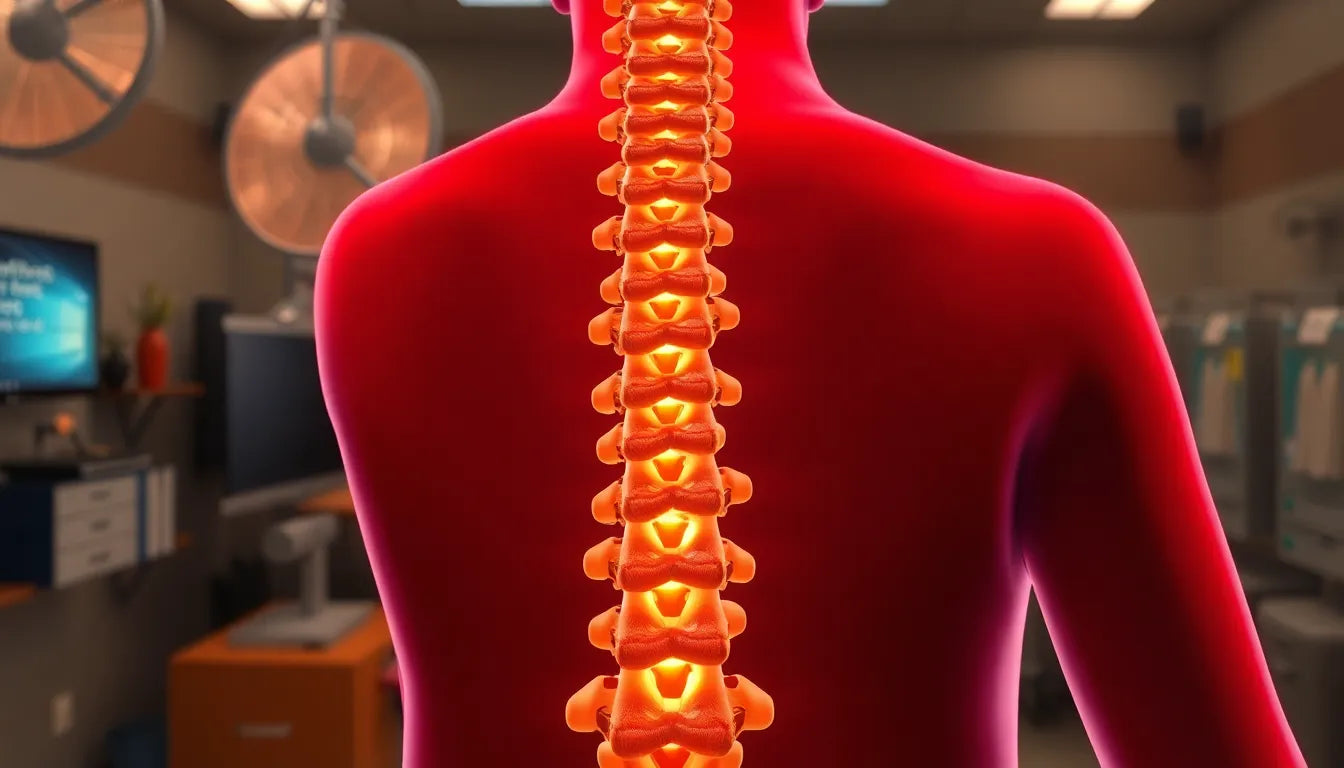
Understanding the complexities of herniated disc pain is crucial for those experiencing this common yet often debilitating condition. A herniated disc, also known as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a tear in its tougher exterior. This can lead to irritation of nearby nerves, resulting in pain, numbness, or weakness in an arm or leg. Addressing herniated disc pain promptly is essential to prevent further complications and to maintain a good quality of life.
Herniated disc pain can manifest in various ways, depending on the location and severity of the herniation. Common symptoms include sharp or dull pain in the lower back, sciatica, tingling, and muscle weakness. These symptoms can significantly impact daily activities, making it difficult to perform even simple tasks. It's important to recognize these signs early and seek appropriate medical advice to manage the condition effectively.
The impact of herniated disc pain on daily life
Living with herniated disc pain can be challenging, as it often affects mobility and overall quality of life. The discomfort can limit one's ability to engage in physical activities, leading to a more sedentary lifestyle. This can have a ripple effect on one's physical health, potentially leading to weight gain and decreased cardiovascular fitness. Furthermore, the prevalence of herniated disc issues is notable, with a significant portion of the adult population experiencing this condition at some point in their lives.
Beyond the physical implications, herniated disc pain can also take an emotional and psychological toll. Chronic pain is known to contribute to feelings of frustration, anxiety, and depression. The constant discomfort and limitations imposed by the condition can affect one's mental well-being, making it crucial to address both the physical and emotional aspects of the pain. Understanding and managing herniated disc pain is not only about alleviating physical symptoms but also about improving overall quality of life and mental health.
Symptoms and diagnosis of herniated disc pain
Herniated disc pain can present a range of symptoms that vary significantly based on the location and severity of the herniation. Commonly, individuals experience lower back pain, which may radiate down the legs, a condition known as sciatica. This can be accompanied by numbness, tingling, and muscle weakness, particularly in the limbs. The specific symptoms depend on which part of the spine is affected. For instance, a herniation in the cervical spine might lead to pain and weakness in the neck, shoulders, and arms, while a lumbar disc herniation often affects the lower back and legs.
Diagnosing a herniated disc typically involves a combination of physical examinations and neurological tests. During a physical exam, a healthcare provider may check for muscle strength, reflexes, and the ability to walk or feel sensations in the limbs. If a herniated disc is suspected, imaging techniques such as MRI scans are often used to confirm the diagnosis. MRI scans provide detailed images of the spine, revealing the presence and extent of disc herniation, thereby guiding the appropriate treatment approach.
Exploring non-surgical treatment options
For many patients, non-surgical treatments are the first line of defense against herniated disc pain. These methods focus on relieving pain and improving function without the need for invasive procedures. Rest and activity modification are often recommended initially to reduce strain on the affected area. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be effective in managing pain and reducing inflammation. Physical therapy is another crucial component, helping to strengthen the muscles around the spine, improve flexibility, and promote proper posture.
In cases where pain is severe, epidural steroid injections may be considered. These injections deliver anti-inflammatory medication directly to the area around the herniated disc, providing significant pain relief for some patients. The benefits of non-surgical treatments include fewer risks and a shorter recovery time compared to surgical options. It is generally advisable to pursue these methods before considering surgery, especially if they effectively manage symptoms and improve quality of life.
When surgery becomes necessary
While non-surgical treatments are effective for many, surgery may be necessary for those who experience persistent pain or severe nerve compression. This is particularly true if there is significant muscle weakness or loss of function in the limbs. Surgical options vary, but common procedures include discectomy, which involves removing the herniated portion of the disc, and spinal fusion, which stabilizes the spine by fusing two or more vertebrae together.
The decision to undergo surgery is typically based on the severity of symptoms and the extent to which they impact daily life. Although surgery carries risks, advances in medical technology have improved outcomes, making these procedures safer and more effective. Patients considering surgery should discuss the potential benefits and risks with their healthcare provider to make an informed decision.
Lifestyle modifications and pain management
Managing herniated disc pain effectively often requires lifestyle modifications alongside medical treatments. Maintaining a healthy weight is crucial, as excess weight can place additional strain on the spine, exacerbating pain. Regular exercise, particularly activities that strengthen the core and improve flexibility, can also help support the spine and prevent further injury. However, it is important to consult with a healthcare provider to ensure that any exercise regimen is appropriate for your specific condition.
Ergonomic improvements in daily activities can significantly reduce strain on the back. This includes setting up a workstation that supports good posture, using chairs with proper lumbar support, and being mindful of lifting techniques to avoid unnecessary pressure on the spine. Additionally, alternative therapies such as acupuncture and chiropractic care may provide relief for some individuals, although their effectiveness can vary. It's advisable to discuss these options with a healthcare professional to determine their suitability.
Long-term outlook and recovery
The recovery timeline for herniated disc pain varies depending on the severity of the condition and the treatments employed. Many individuals experience significant improvement within a few weeks to months with non-surgical treatments. However, for those who undergo surgery, recovery can take longer, often requiring several months of rehabilitation to regain full function.
Consistency and patience are key in the rehabilitation process. Following medical advice and adhering to prescribed treatment plans are essential for optimal recovery and pain management. Engaging in physical therapy and maintaining a healthy lifestyle can support long-term recovery and help prevent future disc issues. It's important to remain positive and committed to the recovery process, as this can greatly influence outcomes.
Frequently asked questions
What causes herniated disc pain?
Herniated disc pain is often caused by aging-related wear and tear on the spine, known as disc degeneration. Physical stress, such as lifting heavy objects improperly or sudden traumatic injuries, can also lead to disc herniation, causing pain and discomfort.
How long does it take for herniated disc pain to heal?
The healing time for herniated disc pain varies. With non-surgical treatments, many people experience relief within a few weeks to months. Surgical intervention may require a longer recovery period, often several months, depending on the individual's health and adherence to rehabilitation.
Can a herniated disc heal on its own?
In some cases, a herniated disc can heal on its own as the body reabsorbs the herniated material over time. However, if symptoms persist or worsen, medical intervention may be necessary to prevent complications and ensure proper recovery.
Are there any exercises to avoid with a herniated disc?
Individuals with a herniated disc should avoid exercises that place excessive strain on the spine, such as heavy lifting, high-impact activities, and certain twisting motions. It's important to consult with a healthcare provider or physical therapist to determine safe exercises tailored to your condition.
What are the risks of not treating a herniated disc?
Failing to treat a herniated disc can lead to chronic pain, worsening symptoms, and potential complications such as permanent nerve damage. Early intervention and appropriate treatment are crucial to prevent these risks and improve quality of life.