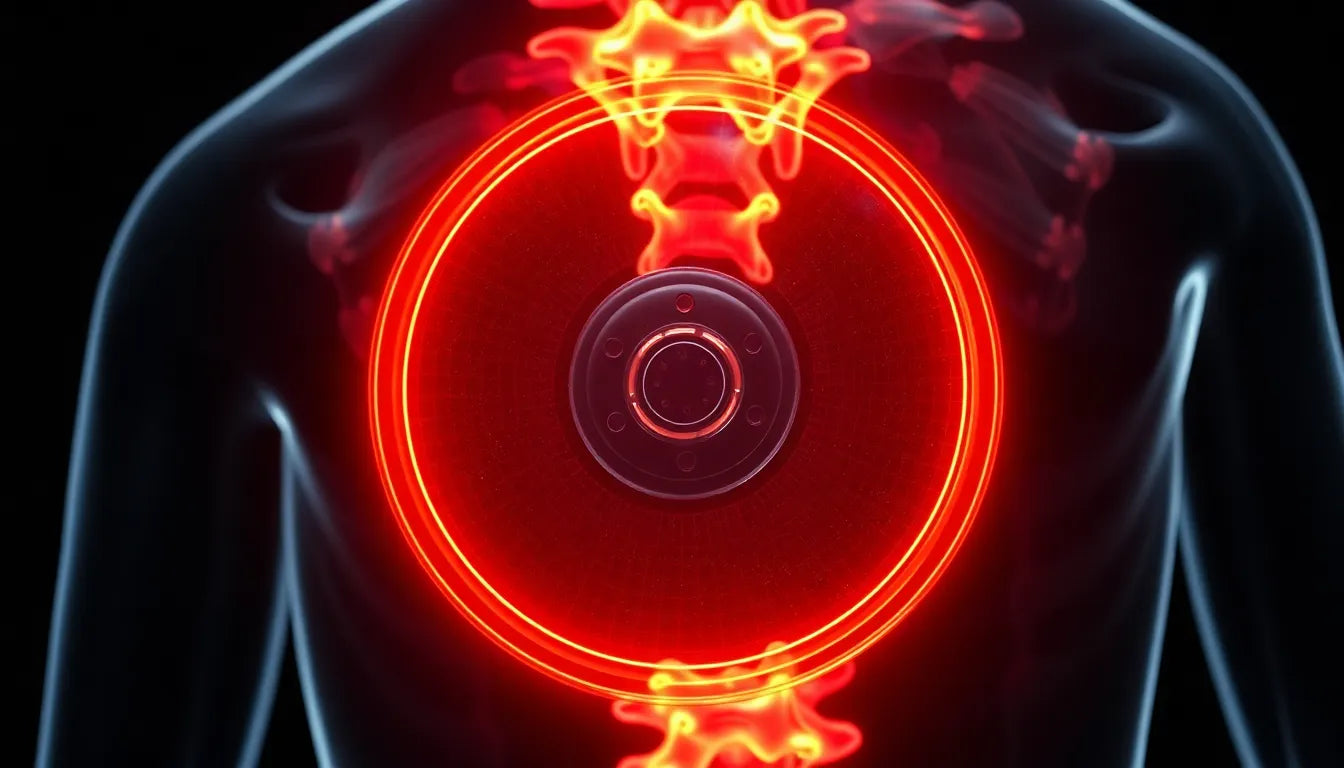
Herniated disc issues are a common affliction that can significantly impact everyday activities, causing discomfort and limiting mobility. As the prevalence of this condition continues to rise, so does the need for effective treatment solutions. Traditionally, surgical intervention has been a daunting prospect for many, often associated with lengthy recovery times and significant discomfort. However, the landscape of surgical treatment is evolving, with minimally invasive techniques now at the forefront, promising quicker recoveries and less disruption to daily life.
understanding herniated discs and the need for surgery
A herniated disc occurs when the soft inner gel of a spinal disc pushes through a crack in the tougher exterior casing. This can irritate nearby nerves, leading to pain, numbness, or weakness in an arm or leg. While many cases can be managed with conservative treatments such as physical therapy, medication, or injections, surgery may become necessary when these methods fail to alleviate symptoms. Traditional surgical options, such as open discectomy, involve removing the damaged portion of the disc to relieve nerve pressure. However, these procedures often come with limitations, including significant recovery times and potential complications.
the purpose of exploring new surgical advancements
The goal of this post is to delve into the latest advancements in herniated disc surgery, particularly focusing on minimally invasive methods. These innovative techniques are transforming the recovery experience for patients, offering substantial benefits over traditional surgery. By exploring these options, we aim to provide valuable insights into how these procedures work, their advantages, and why they are becoming the preferred choice for many patients and healthcare professionals alike.
exploring common surgical procedures for herniated discs
When conservative treatments for a herniated disc fall short, surgical intervention often becomes a viable option. The most commonly performed procedure is the discectomy, which involves removing the damaged portion of the disc to relieve nerve pressure. Traditionally, this procedure required a larger incision and significant tissue disruption, but advancements have led to more refined techniques.
discectomy: traditional vs. partial removal
In a traditional discectomy, surgeons may choose between partial or full disc removal. Partial removal focuses on excising only the protruding section of the disc, which is typically sufficient to alleviate symptoms. This approach maintains more of the disc's structure, potentially reducing the risk of spinal instability. Outcomes of traditional discectomy generally include significant pain relief, but the procedure requires a longer recovery period compared to minimally invasive methods.
microdiscectomy: a minimally invasive approach
Microdiscectomy represents a significant advancement in herniated disc surgery. This minimally invasive technique utilizes smaller incisions and specialized instruments, resulting in less tissue disruption. Patients benefit from a quicker recovery, with many returning to normal activities within a few weeks. Compared to traditional discectomy, microdiscectomy offers similar success rates but with reduced postoperative pain and faster rehabilitation.
endoscopic discectomy: the cutting-edge technique
Endoscopic discectomy is at the forefront of minimally invasive spine surgery. This procedure involves the use of an endoscope—a thin tube equipped with a camera—to access and remove herniated disc material through very small incisions. According to insights from Yale Medicine, endoscopic discectomy is gaining popularity due to its minimal tissue disruption, reduced scarring, and rapid recovery times. Patients often experience less postoperative pain, making it an attractive option for those seeking the least invasive surgical solution.
other surgical options for herniated disc treatment
Beyond discectomy, several other surgical procedures can address herniated discs, each with unique benefits and considerations.
laminotomy and laminectomy: relieving nerve pressure
Laminotomy and laminectomy involve the removal or opening of part of the vertebral bone known as the lamina. This procedure alleviates pressure on the nerve roots, often in conjunction with disc removal. These techniques can be particularly beneficial for patients experiencing severe nerve compression, offering relief from pain and neurological symptoms.
artificial disc replacement: a modern alternative
Artificial disc replacement is a modern surgical option for specific cases, such as single-disc issues in the lower back. This procedure involves replacing the damaged disc with a synthetic one, preserving spinal mobility and potentially reducing the risk of adjacent segment degeneration. However, it is not suitable for everyone, particularly those with arthritis or multi-disc problems.
spinal fusion: stabilizing the spine
Spinal fusion is often considered when other surgical options are not viable. This procedure involves fusing two or more vertebrae together using bone grafts and hardware, providing stability to the spine post-disc removal. While effective in stabilizing the spine, spinal fusion may limit mobility in the affected area.
criteria for considering herniated disc surgery
Surgery for a herniated disc is typically considered when conservative treatments, such as physical therapy, medication, or injections, fail to provide relief after a period of six weeks. Severe symptoms, including significant pain, numbness, weakness, or loss of bladder or bowel control, also warrant surgical consideration. A comprehensive evaluation by a healthcare professional will determine the most appropriate surgical option based on the patient's specific condition and overall health.
In summary, the landscape of herniated disc surgery is evolving, with minimally invasive techniques offering promising outcomes and quicker recoveries. As these advanced procedures continue to revolutionize patient experiences, understanding the various surgical options and their benefits becomes crucial in making informed decisions about treatment.
recovery and outcomes of minimally invasive herniated disc surgery
Minimally invasive techniques, such as microdiscectomy and endoscopic discectomy, are transforming recovery experiences for patients undergoing herniated disc surgery. These procedures are designed to minimize tissue disruption, resulting in quicker recovery times and reduced postoperative pain.
microdiscectomy recovery insights
Microdiscectomy typically offers a swift recovery, with many patients experiencing significant pain relief within a few weeks. According to patient testimonials from the Atlantic Spine Center, individuals often return to normal activities in about 12 weeks, although recovery can vary based on individual health and healing rates. Factors influencing recovery speed include the patient's overall health, adherence to post-surgical care instructions, and the success of the surgery itself.
endoscopic discectomy recovery benefits
Endoscopic discectomy is noted for its even faster recovery times and reduced post-surgical pain. The procedure's minimal invasiveness, characterized by very small incisions and minimal tissue damage, allows patients to resume their daily activities more quickly than traditional methods. The rapid recovery and lessened discomfort make it a preferred choice for many seeking a less invasive surgical option.
general outcomes of minimally invasive surgery
Patients undergoing minimally invasive herniated disc surgery generally report substantial pain relief and improved quality of life. However, outcomes can vary based on factors such as the extent of the herniation, the specific procedure performed, and the patient's health status. While most individuals experience significant improvements, it is essential to follow a tailored recovery plan to ensure optimal results.
trends in minimally invasive herniated disc surgery
The trend towards minimally invasive surgery is gaining momentum, with these techniques offering numerous benefits over traditional methods. These procedures not only reduce recovery time but also minimize the risk of complications, such as infection and scarring. As noted by leading institutions like Mayo Clinic and HSS, patient education and shared decision-making play crucial roles in determining the most appropriate surgical approach. Patients are encouraged to engage in open discussions with their healthcare providers to explore all available options and make informed decisions about their treatment.
frequently asked questions
What is the recovery time for minimally invasive herniated disc surgery?
Recovery time for minimally invasive herniated disc surgery varies but is generally quicker than traditional methods. Microdiscectomy patients often return to normal activities within 12 weeks, while endoscopic discectomy may allow for even faster recovery due to its minimal invasiveness.
How do minimally invasive techniques compare to traditional surgery?
Minimally invasive techniques involve smaller incisions, leading to reduced recovery time and lower risk of complications such as infection and scarring. These methods generally result in less postoperative pain and quicker return to daily activities compared to traditional open surgery.
Who is a candidate for minimally invasive surgery?
Candidates for minimally invasive surgery typically include individuals who have not found relief from conservative treatments and exhibit severe symptoms. Factors such as overall health, specific disc issues, and the presence of other medical conditions are considered when determining candidacy.
What are the risks associated with herniated disc surgery?
While minimally invasive surgery generally poses fewer risks, potential complications include infection, nerve damage, and recurrence of disc herniation. Traditional surgery may carry higher risks due to larger incisions and increased tissue disruption.
When should surgery be considered over conservative treatments?
Surgery is usually considered when conservative treatments, such as physical therapy and medication, fail to alleviate symptoms after six weeks. Severe symptoms, including significant pain, numbness, or loss of bladder or bowel control, also warrant surgical consideration.
Sources
- Mayo Clinic. "Diskectomy and Herniated Disk Treatment."
- Hospital for Special Surgery. "Microdiscectomy Surgery Overview."
- Healthline. "Herniated Disc Surgery Types and Expectations."
- Medical News Today. "Surgery Procedures and Recovery for Herniated Discs."
- Yale Medicine. "Advances in Minimally Invasive Disc Surgery."
- Atlantic Spine Center. "Recovery After Microdiscectomy."