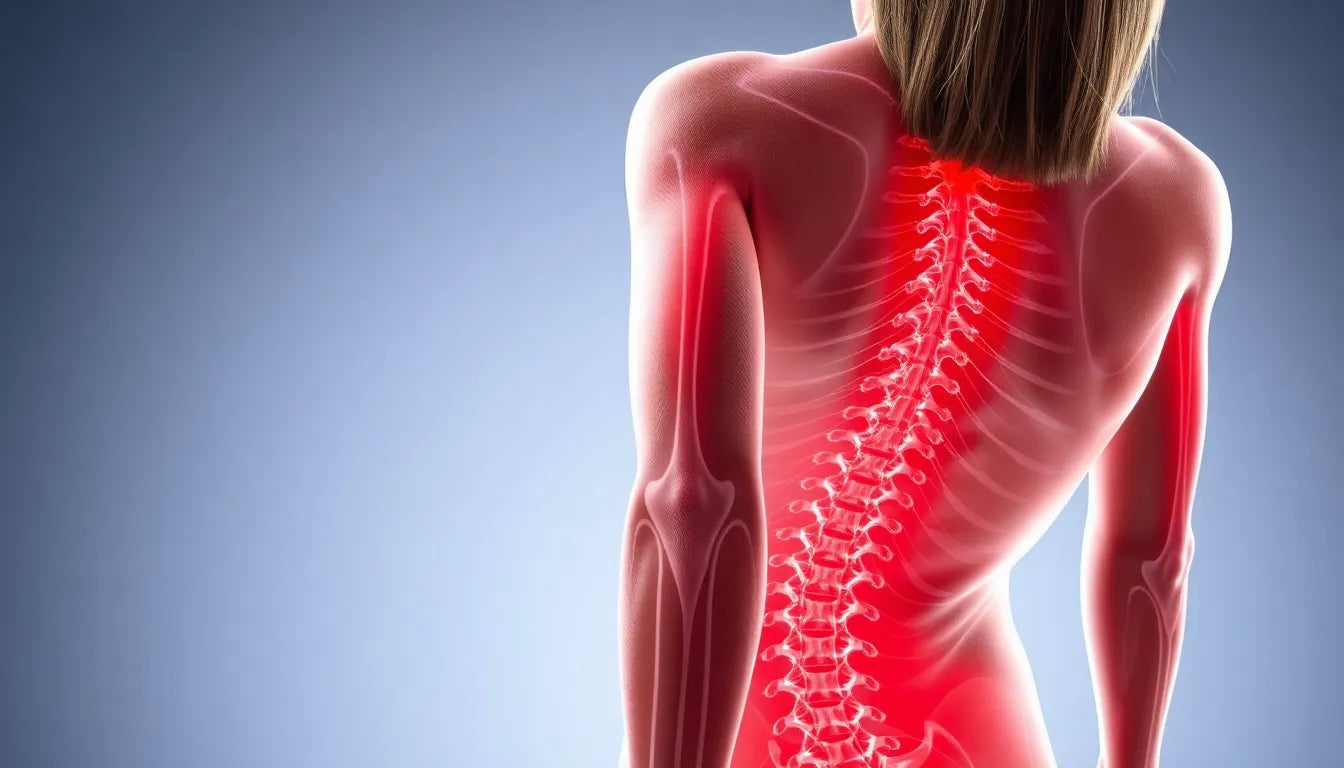
Back pain is an all-too-common ailment that affects millions of people worldwide, often disrupting daily life and complicating even the simplest of tasks. Among the various causes of back pain, herniated discs stand out as a significant contributor. Understanding the nature of herniated discs and how they can be accurately diagnosed is crucial for effective treatment and management. This is where MRI scans come into play, serving as a vital tool in the diagnostic process.
Understanding herniated discs
A herniated disc, sometimes referred to as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a tear in the tougher exterior. This condition can lead to a range of symptoms, including persistent back pain, leg pain, numbness, or tingling in the limbs. In some cases, it may even result in muscle weakness or difficulty controlling certain bodily functions. The severity of these symptoms can vary greatly depending on the location and extent of the herniation.
Accurate diagnosis of a herniated disc is essential to prevent further complications and to tailor an effective treatment plan. Misdiagnosis or delayed diagnosis can lead to prolonged discomfort and potentially exacerbate the condition. Therefore, identifying a herniated disc through reliable diagnostic methods is a critical step in the journey to recovery.
The purpose of this post
The goal of this post is to provide readers with a comprehensive understanding of what a herniated disc looks like on an MRI scan. By exploring the significance of these images in the diagnostic process, we aim to demystify the procedure and highlight its importance. MRI scans are considered the gold standard for diagnosing herniated discs due to their high accuracy and ability to provide detailed images of the spine's internal structures.
Through this post, we will delve into the intricacies of MRI technology, explain how herniated discs appear on these scans, and discuss the specific indicators that medical professionals look for when interpreting the results. Our aim is to empower readers with the knowledge needed to better understand their condition and the diagnostic tools available to them.
In the following sections, we will explore the technical aspects of MRI scans, offer insights into the diagnostic criteria for herniated discs, and discuss scenarios where an MRI might be recommended. By doing so, we hope to bridge the gap between diagnosis and treatment, providing a clearer picture of how MRI scans play a pivotal role in managing herniated disc-related issues.
Understanding mri scans for herniated discs
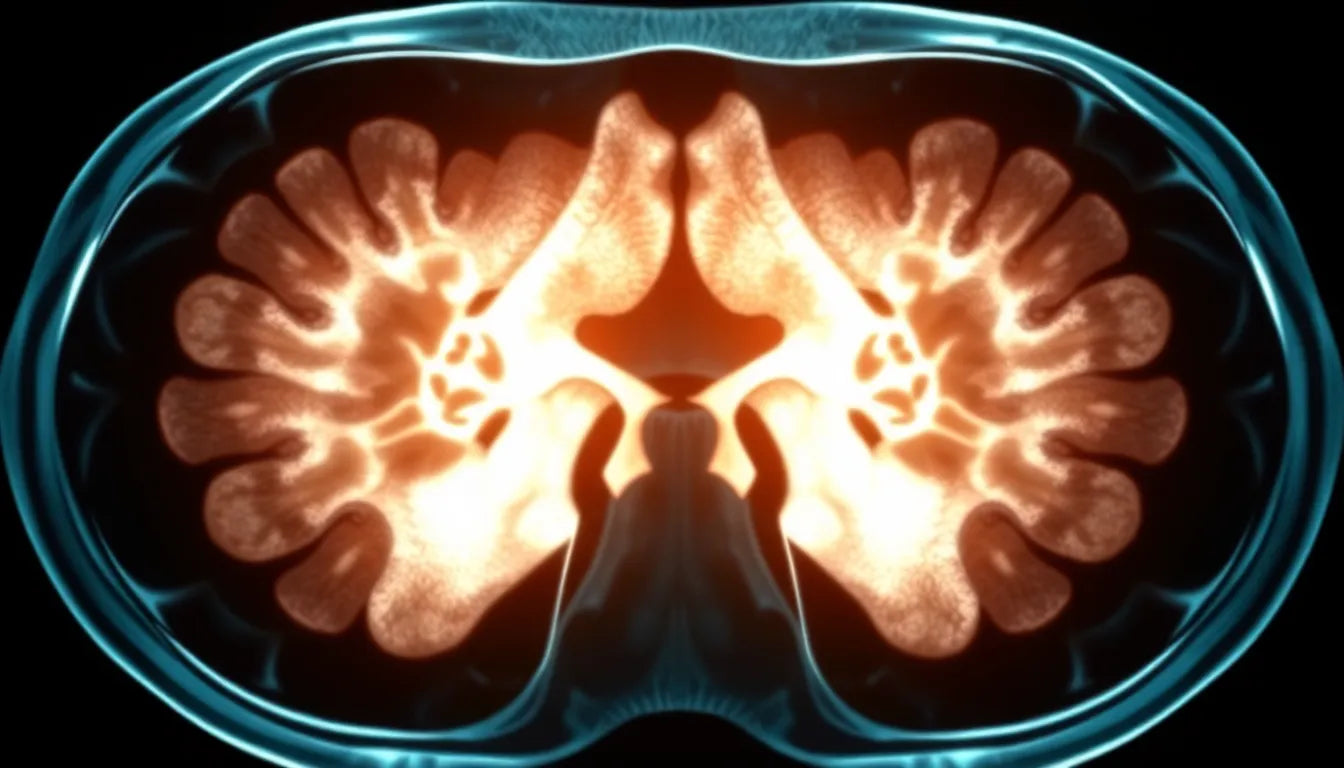
Magnetic Resonance Imaging (MRI) scans are a cornerstone in the diagnosis of herniated discs, offering a non-invasive and highly detailed view of the spine's internal structures. Unlike X-rays or CT scans, which primarily show bones, MRI scans use powerful magnets and radio waves to create detailed images of soft tissues, including discs, muscles, and nerves. This ability to visualize soft tissue makes MRI the gold standard for diagnosing spinal conditions, including herniated discs.
One of the key advantages of MRI scans is their accuracy. Studies have shown that MRI scans have a diagnostic accuracy of 95-97% for identifying herniated discs, making them an invaluable tool for clinicians. This high level of precision is crucial for developing effective treatment plans, as it allows healthcare providers to pinpoint the exact location and extent of the disc herniation.
Visualizing herniated discs on an mri
On an MRI scan, a herniated disc typically appears as a bulging or protruding area of the disc material that extends beyond its normal boundaries. This protrusion can compress nearby nerves, leading to the symptoms commonly associated with herniated discs. Radiologists and doctors look for specific signs such as disc displacement, loss of disc height, and nerve root compression when examining MRI images.
To help visualize this, imagine the spinal disc as a jelly-filled doughnut. When herniation occurs, the "jelly" pushes through a tear in the outer layer, creating a bulge. On an MRI image, this bulge is clearly visible, often appearing as a darker area against the lighter background of the spinal column. A labeled diagram or image of an MRI scan showing a herniated disc can provide a valuable reference for those unfamiliar with these medical images, helping patients better understand their condition.
Diagnostic criteria and indicators
Medical professionals rely on several indicators when diagnosing a herniated disc from an MRI scan. Key criteria include the size and location of the disc protrusion, the degree of nerve compression, and any associated spinal abnormalities. These factors are critical in determining the severity of the condition and the most appropriate treatment options.
Insights from medical experts highlight the importance of a comprehensive assessment. Dr. John Smith, a renowned neurosurgeon, notes, "The precise interpretation of MRI scans is essential for identifying not just the herniation but also understanding its impact on surrounding structures. This understanding guides the clinical decision-making process, ensuring that patients receive the most effective care."
When to consider an mri scan
While not every case of back pain requires an MRI, there are specific scenarios where this diagnostic tool becomes essential. An MRI is recommended when a patient experiences severe pain, neurological symptoms such as numbness or weakness, or when pain persists beyond 6-8 weeks despite conservative treatment. Additionally, MRIs play a crucial role in surgical planning, providing surgeons with a detailed map of the affected area.
In summary, MRI scans are a vital component in the diagnosis and management of herniated discs. Their ability to provide detailed images of the spine's soft tissues allows for accurate diagnosis and informed treatment decisions. Understanding what a herniated disc looks like on an MRI scan empowers patients with the knowledge needed to engage actively in their healthcare journey.
Connecting diagnosis to treatment
Once a herniated disc is diagnosed through an MRI scan, the next step is to determine the most appropriate treatment plan. The findings from the MRI play a crucial role in guiding this decision-making process. For many patients, non-surgical options such as physical therapy, medication, and lifestyle modifications are effective in managing symptoms. Physical therapy often focuses on exercises that strengthen the muscles supporting the spine and improve flexibility.
In cases where conservative treatments do not provide relief, or if the herniation is severe, surgical options may be considered. Procedures such as discectomy or spinal fusion can relieve pressure on the nerves and restore stability to the spine. Regardless of the treatment path, incorporating ergonomic aids, such as supportive chairs or cushions, can enhance comfort and aid recovery.
Cost and insurance considerations
Understanding the financial aspects of obtaining an MRI scan is important for many patients. Costs can vary widely depending on factors such as geographic location, the facility where the scan is performed, and whether the patient has insurance coverage. Below is a summary of potential costs:
| Coverage Type | Estimated Cost |
|---|---|
| Without Insurance | $400 - $12,000 |
| With Insurance | Varies based on deductibles and copayments |
| Medicare Part B | 20% of the Medicare-approved amount after deductibles |
| Medicaid | Typically covers MRIs completely |
Patients are encouraged to consult with their healthcare provider and insurance company to understand their specific coverage and any out-of-pocket expenses they may incur.
Preventative measures
Preventing herniated discs is an important aspect of maintaining spinal health. Proper ergonomics, especially in work and home environments, can significantly reduce the risk of disc herniation. Key preventative measures include maintaining good posture, using ergonomic furniture, and taking regular breaks to stretch and move around.
Investing in supportive equipment, such as ergonomic chairs and lumbar support cushions, can help maintain the natural curve of the spine and distribute weight evenly, reducing stress on the discs. Additionally, engaging in regular physical activity to strengthen core muscles can provide essential support to the spine.
Frequently Asked Questions
What does a herniated disc look like on an MRI?
A herniated disc on an MRI scan typically appears as a bulging or protruding area of the disc material that extends beyond its normal boundaries. This bulge can compress nearby nerves, which is visible as a darker area against the lighter background of the spinal column.
How accurate are MRI scans in diagnosing herniated discs?
MRI scans are highly accurate in diagnosing herniated discs, with a diagnostic accuracy rate of 95-97%. This precision allows healthcare providers to pinpoint the exact location and extent of the disc herniation.
When should I get an MRI for back pain?
An MRI is recommended if you experience severe pain, neurological symptoms such as numbness or weakness, or if pain persists beyond 6-8 weeks despite conservative treatment. It is also essential for surgical planning.
What are the costs associated with an MRI scan?
The cost of an MRI scan can range from $400 to $12,000 without insurance. With insurance, costs vary based on deductibles and copayments. Medicare Part B covers 20% of the approved amount after deductibles, while Medicaid typically covers MRIs completely.
Can ergonomic aids help after a herniated disc diagnosis?
Yes, ergonomic aids such as supportive chairs, cushions, and proper workspace setups can significantly aid in recovery and alleviate pain. They help maintain proper posture and reduce strain on the spine, supporting the healing process.
Sources
- ADR Spine. "Understanding MRI for Herniated Discs."
- Deuk Spine. "Herniated Disc MRI Accuracy and Interpretation."
- Ezra. "The Role of MRI in Diagnosing Herniated Discs."
- Dr. Kevin Pauza. "Clinical Insights into MRI for Spinal Conditions."
- Smith, J. (2022). "The Financial Aspects of MRI Scans for Back Pain."