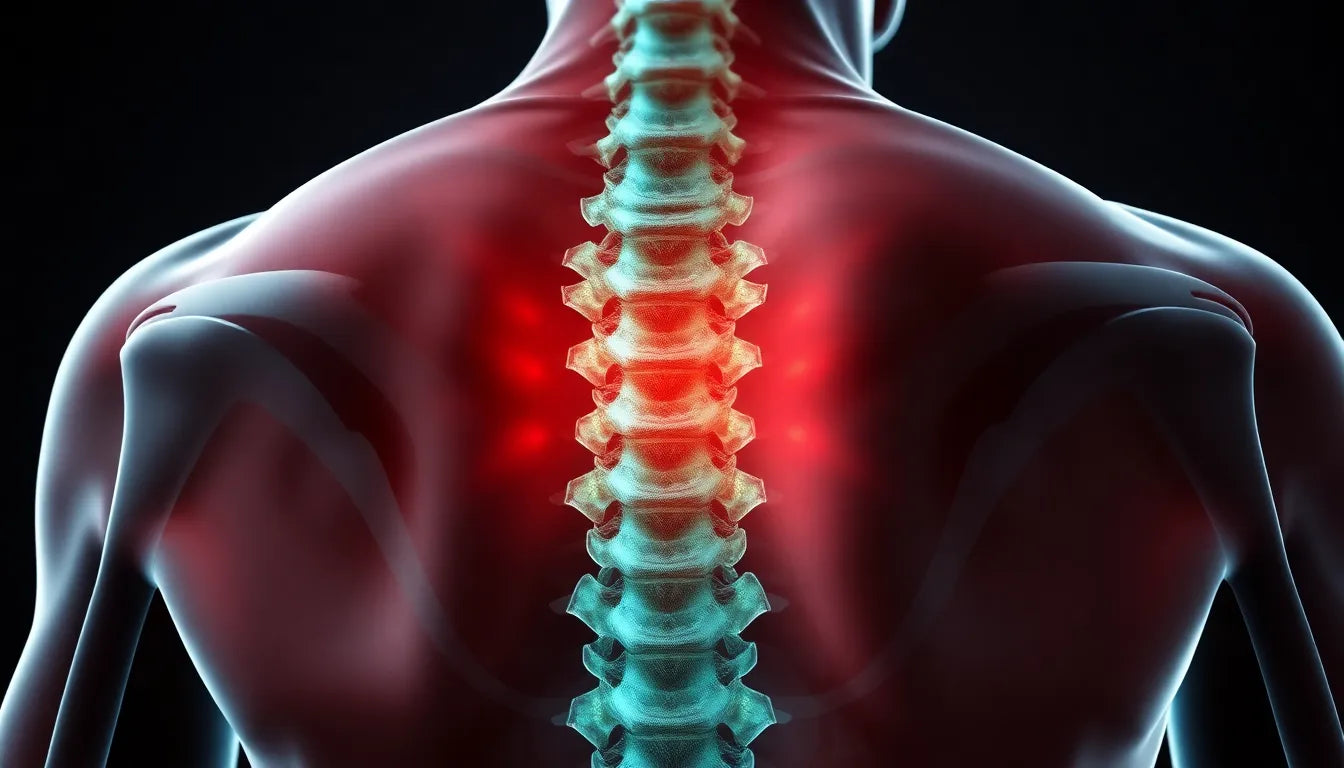
Living with a herniated disc in the lower back can be a challenging experience, often accompanied by persistent pain and discomfort that affects daily activities. A herniated disc occurs when the soft inner gel of a spinal disc pushes through a crack in the tougher exterior casing. This condition frequently impacts the lower back, leading to symptoms such as pain, numbness, and weakness that may extend to the legs. It's a common ailment, especially among adults who either engage in physically demanding jobs or lead a sedentary lifestyle, both of which can contribute to the development of a herniated disc.
the role of surgery in herniated disc treatment
When conservative treatments fail to provide relief, surgery for a herniated disc in the lower back might be considered. This option is generally reserved for cases where symptoms persist despite non-surgical interventions. The primary goal of surgical intervention is to alleviate pain and restore function by removing or repairing the portion of the disc that is pressing on the nerve roots. While the idea of surgery can be daunting, it offers a path to relief for many individuals suffering from severe symptoms.
importance of informed decisions
Before opting for surgery, it's crucial to understand all available treatment options. Surgery is typically considered only after non-surgical methods, such as physical therapy, medications, or injections, have been exhausted. Making an informed decision involves weighing the potential benefits and risks of surgery against the severity of symptoms and their impact on quality of life. By thoroughly exploring all options, individuals can make a choice that aligns with their health goals and lifestyle needs.
types of surgical procedures for herniated discs
When non-surgical treatments for a herniated disc in the lower back prove ineffective, various surgical options are available to alleviate symptoms and restore function. Understanding these procedures can help patients make informed decisions about their treatment paths.
discectomy and microdiscectomy
Discectomy, including its minimally invasive variant microdiscectomy, is one of the most common surgical procedures for addressing herniated discs in the lower back. The primary goal of this surgery is to remove the portion of the disc that's pressing on the nerve roots, which can significantly relieve pain and improve mobility. Microdiscectomy is particularly advantageous due to its use of smaller incisions and specialized instruments, often resulting in quicker recovery times and less postoperative discomfort. Many patients can undergo this procedure on an outpatient basis, allowing them to return home the same day.
lumbar laminotomy and laminectomy
In some cases, surgeons may opt for a laminotomy or laminectomy to access the herniated disc. A laminotomy involves the partial removal of the lamina, the bony arch covering the spinal canal, while a laminectomy entails its complete removal. These procedures are often performed in conjunction with a discectomy to provide better access to the affected area. By relieving pressure on the spinal cord and nerves, these surgeries can alleviate symptoms and improve the patient's quality of life.
spinal fusion
Spinal fusion may be recommended following a discectomy or laminectomy to stabilize the spine. This procedure involves fusing two or more vertebrae together, thereby preventing movement between them and reducing pain. While spinal fusion can be highly effective, it is generally reserved for cases where instability is a concern or when multiple surgeries are needed to address severe disc degeneration.
artificial disc replacement
Artificial disc replacement is a less common surgical option that involves replacing the damaged disc with an artificial one made of metal or plastic. This procedure aims to maintain more natural spine movement compared to spinal fusion. However, it is only suitable for specific cases and requires thorough evaluation by a spine specialist to determine eligibility.
when is surgery recommended for herniated discs?
Surgery for herniated discs in the lower back is typically considered when non-surgical treatments have failed to provide sufficient relief. Candidates for surgery often experience persistent pain, weakness, or tingling that significantly impacts their daily activities, such as sleeping, standing, or walking. These symptoms can be debilitating, making it difficult to maintain a normal lifestyle.
Before opting for surgery, patients are usually encouraged to try a range of non-surgical treatments. These may include physical therapy, which can help strengthen the muscles supporting the spine, epidural steroid injections to reduce inflammation, and anti-inflammatory medications to alleviate pain. Only after these options have been exhausted and symptoms persist is surgery considered a viable option.
Ultimately, the decision to undergo surgery should be made in consultation with a healthcare professional who can assess the severity of symptoms and determine the most appropriate treatment plan. By understanding the various surgical procedures available and the criteria for surgery, patients can make informed decisions that align with their health goals and lifestyle needs.
surgery efficacy and recovery
Undergoing surgery for a herniated disc in the lower back can be a significant step towards relief and improved quality of life. For many patients, the outcomes are promising, with a typical recovery timeline of one to three weeks for those undergoing microdiscectomy. This procedure often results in immediate pain relief, as the pressure on the nerve roots is alleviated. However, it's important to note that while many patients experience a significant reduction in symptoms, residual effects such as leg pain or weakness may take longer to resolve, sometimes extending over several weeks or months.
The minimally invasive nature of procedures like microdiscectomy offers additional benefits, including reduced postoperative pain and quicker recovery times. These advantages make it possible for many patients to resume their normal activities sooner than with traditional surgical methods. The smaller incisions and use of specialized instruments contribute to less tissue damage and a shorter hospital stay, often allowing patients to return home the same day.
frequently asked questions
What are the risks associated with herniated disc surgery?
Like any surgical procedure, herniated disc surgery carries certain risks. Common risks include infection, bleeding, and nerve damage. However, these complications are relatively rare, and surgeons take extensive precautions to minimize them. Discussing potential risks with your surgeon can provide a clearer understanding of what to expect and how to prepare for surgery.
How long does it take to return to normal activities post-surgery?
The timeline for returning to normal activities varies depending on the type of surgery and individual recovery rates. Generally, patients who undergo microdiscectomy can expect to return to light activities within a few weeks. More strenuous activities, such as heavy lifting or high-impact sports, may require a longer recovery period, often several months. It's important to follow your surgeon's specific recommendations to ensure a safe and effective recovery.
What can I do to prevent future herniated discs?
Preventing future herniated discs involves adopting lifestyle changes that support spinal health. Maintaining a healthy weight, practicing good posture, and engaging in regular exercise are essential steps. Strengthening the core muscles can provide better support for the spine, reducing the risk of disc herniation. Additionally, avoiding smoking and using proper techniques when lifting heavy objects can further protect your back.
Are there alternatives to surgery if my symptoms are mild?
If your symptoms are mild, non-surgical treatments may be effective. Options include physical therapy, which can help improve strength and flexibility, as well as epidural steroid injections to reduce inflammation. Anti-inflammatory medications can also alleviate pain and discomfort. It's crucial to consult with a healthcare professional to determine the best approach based on your specific condition and symptoms.
How do I choose the right surgeon for my procedure?
Choosing the right surgeon is a critical step in ensuring a successful outcome. Look for a qualified and experienced spine surgeon by checking their credentials and board certifications. Seeking recommendations from your primary care physician or other healthcare providers can also be helpful. Additionally, reading patient reviews and testimonials can provide insight into the surgeon's expertise and patient care approach.
In conclusion, understanding the surgical options for herniated discs in the lower back, along with their risks and benefits, empowers patients to make informed decisions about their health. By considering both surgical and non-surgical treatments, individuals can choose the path that best aligns with their needs and lifestyle goals.
Sources
- Spine-Health. (2023). "Microdiscectomy (Microdecompression) Spine Surgery."
- Mayo Clinic. (2023). "Herniated Disk: Diagnosis and Treatment."
- Johns Hopkins Medicine. (2023). "Spinal Fusion."
- American Academy of Orthopaedic Surgeons. (2023). "Microdiscectomy."
- Cedars-Sinai. (2023). "Herniated Disk."
- University of Michigan Health. (2023). "Herniated Disc."
- Cleveland Clinic. (2023). "Laminectomy."
- WebMD. (2023). "Herniated Disc Surgery."