Dealing with a herniated disc can be a daunting experience, especially when it impedes your ability to stand up straight. The frustration and discomfort associated with this condition are all too familiar for many individuals who find their daily lives disrupted by the pain and mobility issues that accompany a herniated disc. This common spinal ailment can significantly impact your quality of life, making even the simplest tasks seem insurmountable.
understanding the complexity of herniated discs
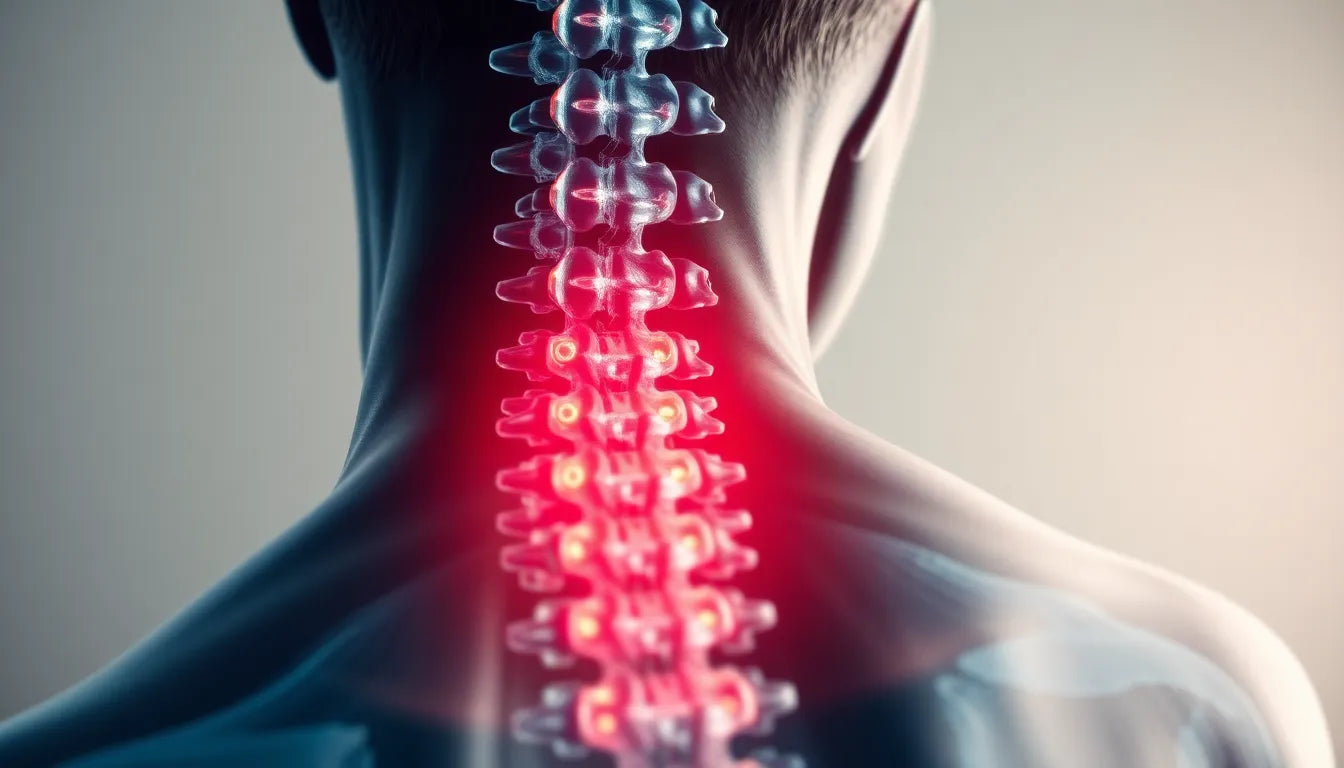
A herniated disc occurs when the soft inner gel of a spinal disc pushes through a tear in the tougher exterior. This condition is prevalent and can affect any part of the spine, but it most commonly occurs in the lower back. The spine's role is crucial in supporting the body's weight and facilitating movement, and when a disc becomes herniated, it can hinder these functions. The resulting pressure on nearby nerves often leads to significant pain, numbness, and muscle weakness, making it difficult to maintain an upright posture.
Standing up straight becomes a challenge because the herniated disc presses on the nerves that control your muscles, leading to spasms and weakness. This not only causes discomfort but also affects your balance and coordination, further complicating your ability to stand or walk without pain.
purpose of this post
This blog post aims to provide a comprehensive understanding of the challenges posed by a herniated disc, particularly why it can make standing up straight so difficult. We will delve into the symptoms and causes of this condition, offering insights into how it affects your body. Additionally, we will explore potential solutions and management strategies to help alleviate the discomfort and improve your mobility. Whether you're experiencing mild discomfort or severe pain, understanding the intricacies of a herniated disc is the first step towards finding relief and regaining your ability to stand tall.
symptoms and warning signs of a herniated disc
Understanding the symptoms of a herniated disc is crucial for anyone experiencing difficulty standing up straight. Common symptoms include persistent pain, numbness, and muscle weakness, which can significantly impact your ability to maintain an upright posture. The pain often radiates from the affected area of the spine to other parts of the body, such as the legs or arms, depending on the location of the herniated disc. This nerve pain can be particularly debilitating, making even the simplest movements challenging.
Muscle spasms are another common symptom and can be a direct result of the disc pressing on nearby nerves. These spasms can cause sudden, involuntary contractions that lead to sharp pain and further hinder your ability to stand or walk comfortably. According to the Miami Neuroscience Center, lumbar herniated discs are particularly problematic, as they can cause poor coordination and cramping in the lower back or legs, exacerbating the difficulty in standing up straight.
unexpected and severe symptoms
While many symptoms of a herniated disc are manageable, some require immediate medical attention. Severe symptoms such as electric shock sensations, significant leg weakness, or foot drop can indicate more serious nerve damage. In rare cases, conditions like myelopathy, characterized by spinal cord compression, can arise, leading to severe balance and walking issues. New York City Spine highlights the importance of recognizing red-flag symptoms such as incontinence or saddle anesthesia, which may signal cauda equina syndrome, a medical emergency that demands prompt intervention.
comparative analysis with other spinal conditions
It's essential to differentiate a herniated disc from other spinal conditions, such as spinal stenosis, to ensure proper treatment. Both conditions can cause similar symptoms, including pain, numbness, and weakness, but they have distinct causes and treatment approaches. Spine.md notes that while both conditions can make standing difficult, spinal stenosis often results from narrowing of the spinal canal, whereas a herniated disc involves the displacement of disc material. Understanding these differences can help in obtaining an accurate diagnosis and effective treatment plan.
biomechanics and posture: why standing is a challenge
The biomechanics of a herniated disc explain why standing up straight can be so challenging. The disc's pressure on spinal nerves leads to nerve impingement, causing pain and muscle weakness. This nerve impingement disrupts the normal function of the muscles that support your spine, leading to spasms and an inability to maintain proper posture. Muscle spasms can force the body into awkward positions, making it physically difficult to stand upright.
To visualize this, imagine a diagram showing the spine's alignment with a herniated disc. The disc's bulge presses against the nerve roots, disrupting the natural curve of the spine and causing a compensatory posture. This misalignment not only increases pain but also affects balance and coordination, further complicating efforts to stand or walk comfortably.
Addressing these biomechanical challenges involves a combination of medical intervention, physical therapy, and ergonomic adjustments. By understanding the underlying mechanics, individuals can take proactive steps to manage their symptoms and improve their ability to stand tall once again.
Recovery and management: finding relief from herniated disc challenges
Understanding the recovery process for a herniated disc is crucial for managing expectations and planning an effective treatment strategy. According to the Cleveland Clinic, many herniated discs improve over time, with a typical recovery period ranging from 4 to 6 weeks. During this time, symptoms such as pain, numbness, and muscle weakness may gradually decrease as the body heals.
For those seeking relief, practical self-care tips can make a significant difference. Incorporating ergonomic solutions into your daily routine can help alleviate discomfort and support recovery. Consider using lumbar supports, seat cushions, or standing desks to maintain proper posture and reduce strain on your spine. Gentle stretching exercises, as recommended by healthcare professionals, can also improve flexibility and strength, aiding in the recovery process.
When to seek professional help
While many herniated discs resolve with conservative treatment, it is important to know when to seek professional help. If symptoms persist or worsen despite self-care efforts, consulting a healthcare provider is crucial. Persistent pain, significant leg weakness, or severe symptoms such as incontinence or saddle anesthesia require immediate medical evaluation. These red-flag symptoms may indicate complications that necessitate prompt intervention to prevent further damage.
frequently asked questions
What causes a herniated disc to make it difficult to stand up straight?
The difficulty in standing up straight with a herniated disc is primarily due to nerve pain, muscle weakness, and spasms. The herniated disc presses on nearby nerves, leading to discomfort and impaired muscle function, which affects posture and balance.
How can I alleviate the pain from a herniated disc at home?
To alleviate pain from a herniated disc at home, consider resting and applying ice or heat to the affected area. Ergonomic aids, such as lumbar supports and seat cushions, can help maintain proper posture. Additionally, gentle stretching exercises can improve flexibility and reduce muscle tension.
When should I see a doctor for my herniated disc?
You should see a doctor if you experience severe symptoms such as incontinence, significant leg weakness, or persistent pain that does not improve with self-care measures. These symptoms may indicate complications that require medical attention.
Can a herniated disc heal on its own?
Yes, many herniated discs improve over time with conservative treatment. However, it is important to seek medical evaluation if symptoms are severe or do not improve, as professional guidance can ensure proper management and recovery.
By understanding the recovery process and knowing when to seek professional help, individuals can effectively manage the challenges of a herniated disc. Combining self-care strategies with medical advice can lead to significant improvements, helping you find relief and stand tall once again.
Sources
- Miami Neuroscience Center. "Understanding Herniated Discs and Their Symptoms."
- Penn Medicine. "Symptoms and Diagnosis of Herniated Discs."
- CORE Orthopedics. "Unexpected Symptoms of Herniated Discs."
- Cleveland Clinic. "Herniated Disc Overview and Recovery."
- New York City Spine. "Red-Flag Symptoms of Herniated Discs."
- Spine.md. "Comparing Herniated Discs with Other Spinal Conditions."