Living with a herniated disc can be an overwhelming challenge, affecting every aspect of daily life. This condition, characterized by the protrusion of a spinal disc's soft center through its tougher exterior, often leads to significant discomfort and pain. It's a common issue that many people face, disrupting normal activities and reducing quality of life. This blog post aims to provide comprehensive insights into effectively managing a herniated disc, guiding you on a path to pain-free living.
understanding a herniated disc
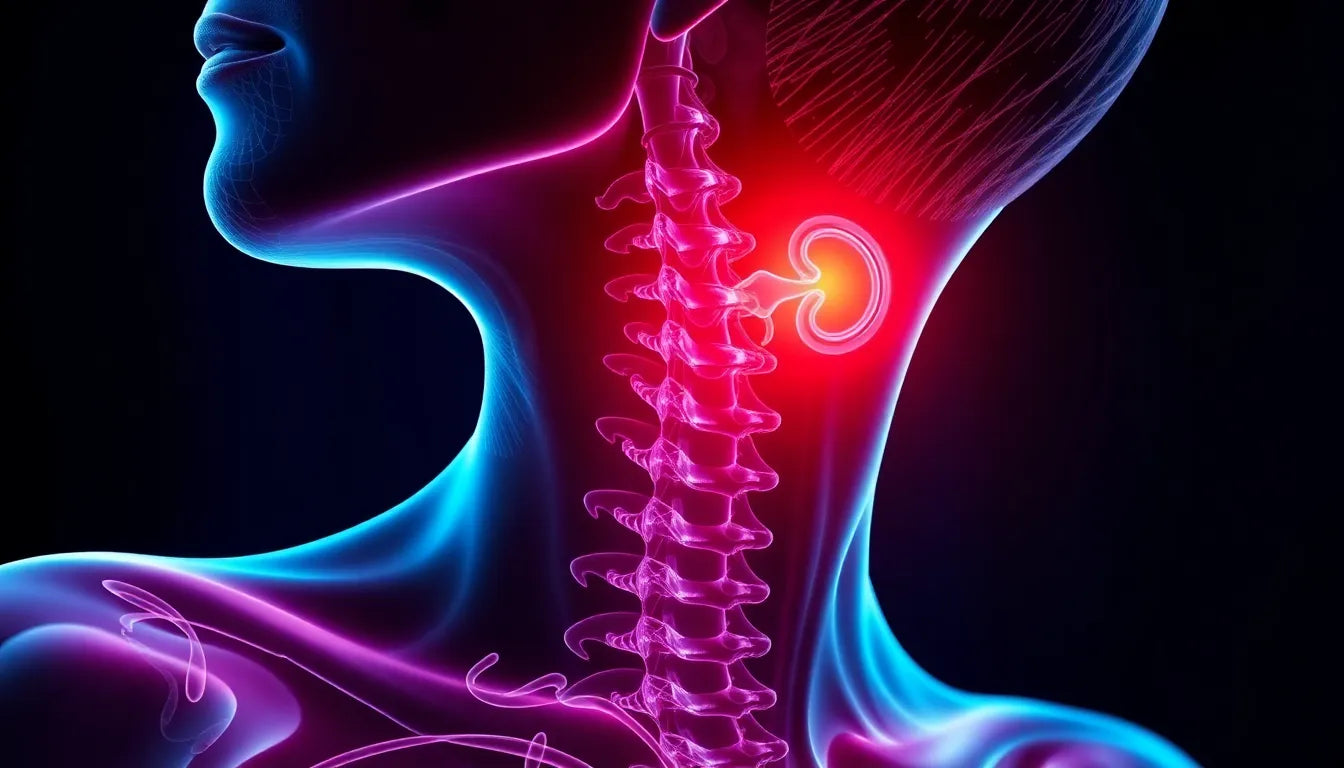
A herniated disc, sometimes referred to as a slipped or bulging disc, occurs when the inner gel-like core of a spinal disc pushes through a crack in its outer layer. This can happen due to several reasons, including age-related degeneration, injury, or excessive strain on the spine. As we age, our spinal discs lose some of their water content, making them less flexible and more prone to tearing or rupturing. This condition can put pressure on nearby nerves, resulting in pain, numbness, or weakness in the back, neck, arms, or legs.
common symptoms and initial concerns
The symptoms of a herniated disc can vary depending on the location of the disc and the nerves affected. Common signs include sharp or shooting pain that radiates to the buttocks, legs, or arms, accompanied by numbness or tingling in these areas. Muscle weakness is another frequent symptom, potentially affecting your ability to perform everyday tasks. In some cases, individuals may not experience any symptoms at all, making it crucial to pay attention to any unusual sensations or discomfort.
Recognizing the symptoms early is essential to prevent further complications. If left untreated, a herniated disc can lead to chronic pain and even permanent nerve damage. Therefore, understanding the warning signs and seeking medical advice promptly can make a significant difference in managing the condition effectively.
In the following sections, we will delve deeper into the diagnosis process, explore various treatment options, and discuss lifestyle adjustments that can aid in recovery and long-term relief. By understanding the intricacies of a herniated disc, you can take proactive steps towards a healthier, pain-free life.
diagnosing a herniated disc: identifying the problem
Accurately diagnosing a herniated disc is crucial for effective management and treatment. The process typically begins with a thorough physical examination by a healthcare professional, who will assess reflexes, muscle strength, and sensory function. This hands-on evaluation helps determine the extent of nerve involvement and the specific location of the disc issue.
For a more detailed view, imaging studies are often employed. X-rays can rule out other causes of back pain, while more advanced imaging techniques like CT scans and MRIs provide a clearer picture of the spinal structures. These tools allow doctors to see the exact position of the herniated disc and its effect on surrounding nerves. In complex cases, nerve testing such as electromyography (EMG) and nerve conduction studies may be used to assess the electrical activity of muscles and the speed of nerve signals, offering additional insights into nerve damage or irritation.
conservative treatment options for herniated discs
In many cases, herniated discs can be managed effectively through conservative treatment approaches, allowing individuals to avoid surgical interventions. One of the primary strategies is activity modification, which involves adjusting daily routines to minimize strain on the spine. This might include avoiding heavy lifting, bending, or twisting movements that could exacerbate symptoms.
Physical therapy plays a pivotal role in the recovery process. A tailored exercise program designed by a physical therapist can help strengthen the muscles supporting the spine, improve flexibility, and reduce pain. Techniques such as stretching, stabilization exercises, and posture training are commonly used to enhance the spine's function and prevent future injuries.
Pain management is another critical component of conservative treatment. Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate mild to moderate discomfort. For more severe pain, doctors may prescribe stronger medications, including muscle relaxants or corticosteroid injections, to reduce inflammation and provide relief.
exploring alternative therapies for herniated disc relief
Beyond traditional treatments, alternative therapies can offer additional relief and support recovery. Rehabilitation and physical therapy modalities such as traction, massage, and heat/cold therapy can be effective in reducing pain and promoting healing. Techniques like ultrasound and electrical muscle stimulation are also employed to enhance blood flow and reduce muscle tension.
Complementary approaches like yoga and Pilates are gaining popularity as they focus on improving core strength, flexibility, and overall body awareness. These practices can be particularly beneficial in managing symptoms and preventing recurrence. Massage therapy is another option that can help alleviate muscle tension and improve circulation, contributing to a sense of well-being.
when surgery becomes necessary
While most herniated discs can be managed with conservative treatments, surgery may be necessary in certain situations. If a patient experiences persistent pain, significant neurological deficits, or if conservative methods fail to provide relief, surgical intervention might be considered. Common surgical options include discectomy, where the protruding portion of the disc is removed, or in some cases, artificial disc replacement, which involves replacing the damaged disc with an artificial one.
The decision to proceed with surgery is made on a case-by-case basis, taking into account the severity of symptoms, the patient's overall health, and the potential benefits and risks of the procedure. It's essential for individuals to discuss all available options with their healthcare provider to make an informed decision about their treatment plan.
As we continue, we will explore lifestyle adjustments that can support long-term relief and delve into patient stories that offer hope and inspiration for those navigating the challenges of living with a herniated disc.
lifestyle adjustments for long-term relief from a herniated disc
Living with a herniated disc requires thoughtful lifestyle adjustments to ensure long-term relief and prevent recurrence. One of the most effective strategies is to incorporate ergonomic solutions into your daily routine. This includes using chairs that support proper posture and adjusting your workspace to reduce strain on your back. Simple changes like setting your computer monitor at eye level and using a footrest can make a significant difference.
Posture plays a crucial role in managing a herniated disc. Practicing good posture, whether sitting, standing, or walking, helps alleviate pressure on the spine. Regularly taking breaks to stretch and move around during prolonged periods of sitting can also aid in maintaining spinal health.
Maintaining a healthy weight is another essential factor in managing a herniated disc. Excess weight can put additional pressure on the spine, exacerbating symptoms. A balanced diet combined with regular physical activity can help achieve and maintain a healthy weight, reducing stress on the back.
inspiring patient stories
Hearing from individuals who have successfully managed their herniated disc can provide encouragement and motivation. For instance, Jane, a 45-year-old office worker, found relief through a combination of physical therapy and lifestyle adjustments. By incorporating regular exercise, maintaining a healthy weight, and practicing yoga, she was able to regain her quality of life.
Similarly, Mark, a 50-year-old construction worker, avoided surgery by adhering to a structured physical therapy program and making ergonomic modifications at work. His commitment to following medical advice and making necessary lifestyle changes allowed him to return to his job pain-free.
frequently asked questions
What causes a herniated disc?
A herniated disc can result from age-related degeneration, injury, or excessive strain on the spine. As we age, spinal discs lose water content, making them more susceptible to tearing or rupturing. Activities that involve heavy lifting, twisting, or sudden movements can also contribute to the development of a herniated disc.
How long does it take for a herniated disc to heal?
The healing timeline for a herniated disc varies depending on the severity of the condition and individual factors. Many people experience relief within a few weeks to a few months with conservative treatment. However, some cases may take longer to heal, especially if complications arise.
Can a herniated disc heal on its own?
Yes, in many cases, a herniated disc can heal on its own over time. The body can absorb the protruding material, reducing pressure on the affected nerves. However, it's crucial to monitor symptoms and seek medical attention if they persist or worsen.
What activities should be avoided with a herniated disc?
To prevent aggravating a herniated disc, it's advisable to avoid activities that involve heavy lifting, bending, twisting, or high-impact movements. Instead, focus on low-impact exercises like walking, swimming, or cycling, which can help maintain fitness without stressing the spine.
Is surgery always required for a herniated disc?
Surgery is not always necessary for a herniated disc. Most cases can be managed effectively with conservative treatments such as physical therapy, pain management, and lifestyle adjustments. Surgery is typically considered a last resort when other treatments fail to provide relief or if significant neurological deficits occur.
Sources
- Mayo Clinic. "Herniated Disk."
- Cleveland Clinic. "Herniated Disc: Symptoms, Causes, and Treatment."
- Johns Hopkins Medicine. "Herniated Disk."
- American Association of Neurological Surgeons. "Herniated Disc."
- Cuellar Spine. "Herniated Disc: Causes and Treatments."
- NewYork-Presbyterian. "Herniated Disc."