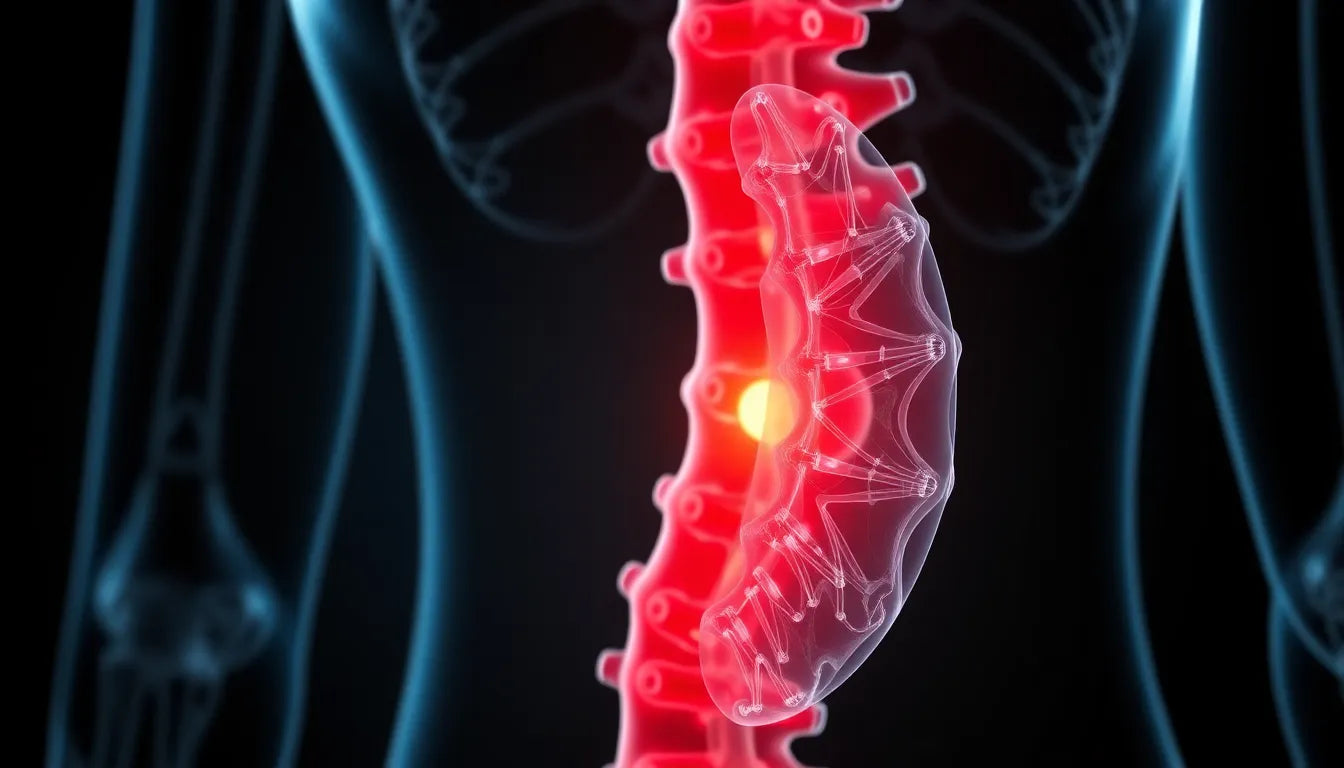
The thoracic spine, often overlooked compared to its cervical and lumbar counterparts, plays a crucial role in the body's overall function. Situated in the middle back, this segment of the spine is responsible for providing stability and supporting the rib cage, which protects vital organs. A herniated disc in this region, known as thoracic disc herniation, occurs when the disc material displaces and presses against nearby nerves. Although less common than herniations in the neck or lower back, thoracic herniations present unique challenges and symptoms that can significantly impact daily life.
Understanding thoracic disc herniation
Thoracic disc herniations are distinct due to the relatively rigid structure of the middle back. This rigidity offers stability but also means that when a disc herniates, the symptoms can be particularly pronounced. Unlike cervical and lumbar herniations, which are more flexible and mobile, thoracic herniations often result in localized pain that can radiate along the ribs or chest wall. This condition can lead to discomfort and a range of symptoms that affect one's quality of life.
The impact of a herniated disc in the middle back
Living with a herniated disc in the middle back can be challenging. Common symptoms include localized pain, radiating pain, numbness, and in severe cases, myelopathy. Myelopathy, a condition involving spinal cord compression, can result in difficulty walking, loss of coordination, and even bowel or bladder dysfunction. These symptoms not only cause physical discomfort but can also limit daily activities and reduce overall mobility.
To illustrate the impact, consider a statistic: approximately 1 in 1,000 individuals will experience a thoracic disc herniation at some point in their lives. While this may seem rare, those affected often find that the condition significantly hampers their ability to perform everyday tasks. For example, simple actions like reaching for an item on a shelf or sitting at a desk for extended periods can become painful and difficult.
Understanding the nature of a herniated disc in the middle back is the first step toward finding relief. By recognizing the symptoms and the unique challenges posed by thoracic disc herniations, individuals can seek appropriate treatment and make informed decisions about their health. In the following sections, we will explore the causes, symptoms, and potential treatment options to help those affected by this condition find the relief they need.
Causes of thoracic disc herniation
Understanding the underlying causes of a herniated disc in the middle back is crucial for both prevention and treatment. Thoracic disc herniation can result from several factors, with trauma or injury being one of the primary causes. Sudden impacts, such as those experienced in car accidents or falls, can exert excessive force on the spine, leading to disc displacement. Additionally, degenerative disc disease, a condition where the discs naturally wear down over time, can also contribute to herniation. This degeneration often stems from the aging process, but it can be accelerated by factors such as poor posture and lifestyle habits.
Another significant contributor is prolonged poor posture, particularly in individuals who spend extended periods sitting or standing with improper alignment. Over time, this can place undue stress on the thoracic spine, weakening the discs and increasing the risk of herniation. To better understand the differences between thoracic, lumbar, and cervical herniations, consider the following table:
| Region | Common Causes |
|---|---|
| Thoracic | Trauma, degenerative disc disease, poor posture |
| Lumbar | Heavy lifting, age-related degeneration, obesity |
| Cervical | Neck injury, repetitive motion, age-related wear |
Symptoms and diagnosis of thoracic herniation
The symptoms of a herniated disc in the middle back can vary, but they typically include localized pain that may radiate along the ribs or into the chest. This pain pattern can sometimes mimic cardiac issues, making accurate diagnosis essential. Neurological symptoms, such as numbness, tingling, or even weakness in the lower limbs, can occur if the herniation affects nerve roots or the spinal cord. In severe cases, myelopathy can develop, leading to impaired coordination and motor function.
Diagnosing a thoracic herniation involves a combination of imaging and physical assessments. MRI scans are particularly effective in visualizing soft tissue structures, allowing for a clear view of the herniated disc and any potential nerve compression. CT scans may also be used to provide detailed images of the spine's bony architecture. Alongside imaging, a thorough physical examination and neurological assessment help pinpoint the affected areas and evaluate the extent of nerve involvement.
Non-surgical treatment options for thoracic disc herniation
For many individuals, non-surgical treatments can effectively manage the symptoms of a herniated disc in the middle back. Rest and activity modification are often the first steps, allowing the affected area to heal while minimizing further strain. Physical therapy plays a crucial role in rehabilitation, focusing on exercises that strengthen the back and core muscles to support the spine and improve posture.
Pain management is another critical component, with non-steroidal anti-inflammatory drugs (NSAIDs) and steroid injections commonly used to reduce inflammation and alleviate discomfort. Additionally, hot and cold therapy can be beneficial, providing relief through alternating temperatures to soothe sore muscles and reduce swelling. Manual manipulation, such as chiropractic adjustments, may also be considered to improve spinal alignment and mobility.
Incorporating specific exercises into a daily routine can further alleviate symptoms and enhance recovery. Consider the following exercises:
- Thoracic extension: Lie on your stomach with your arms at your sides, gently lifting your chest off the ground to extend the spine.
- Cat-cow stretch: On hands and knees, alternate between arching your back upwards and dipping it downwards to mobilize the spine.
- Seated rows: Using a resistance band, pull the band towards your torso while keeping your back straight to strengthen upper back muscles.
These exercises, combined with a comprehensive treatment plan, can significantly improve the quality of life for those dealing with a herniated disc in the middle back. By addressing both the symptoms and underlying causes, individuals can work towards long-term relief and spinal health.
Surgical interventions for herniated discs in the middle back
While many individuals find relief from a herniated disc in the middle back through non-surgical methods, there are cases where surgery becomes necessary. Persistent pain that does not respond to conservative treatments, or the presence of significant neurological deficits such as spinal cord compression, may warrant surgical intervention. The goal of surgery is to alleviate pressure on the nerves, restore function, and improve quality of life.
Two common surgical procedures for thoracic disc herniation are discectomy and spinal fusion. A discectomy involves removing the herniated portion of the disc to relieve nerve compression. In some cases, spinal fusion may be performed to stabilize the affected vertebrae, which involves joining two or more vertebrae together using bone grafts or metal hardware. Recovery from these surgeries varies, but many patients experience significant pain relief and improved mobility. Post-surgery rehabilitation, including physical therapy, is crucial to aid recovery and prevent future issues.
Lifestyle and ergonomic adjustments
Preventing further injury and managing symptoms of a herniated disc in the middle back can be significantly aided by lifestyle and ergonomic adjustments. Setting up an ergonomic workspace is essential for those who spend long hours sitting. This includes using a chair that supports the natural curve of the spine, positioning the computer screen at eye level, and ensuring that feet rest flat on the floor or on a footrest.
In addition to workspace adjustments, incorporating core strengthening and posture correction exercises into daily routines can help maintain spinal health. Exercises such as planks and bridges strengthen the core muscles that support the spine, while posture correction exercises, like chin tucks and shoulder blade squeezes, promote proper alignment.
Maintaining a healthy weight through regular physical activity and a balanced diet can also reduce the strain on the spine and discs. Activities such as swimming, walking, and yoga are excellent for promoting overall fitness without placing excessive stress on the spine.
Frequently asked questions
What is the difference between a herniated and bulging disc?
A herniated disc occurs when the inner gel-like core of the disc pushes through a tear in the outer layer, often compressing nearby nerves. A bulging disc, on the other hand, involves the disc protruding outward without a complete tear. While both conditions can cause pain and discomfort, herniated discs are more likely to cause significant nerve irritation.
Can a herniated disc in the middle back heal on its own?
Yes, many herniated discs in the middle back can heal naturally over time, especially with appropriate conservative treatment. Rest, physical therapy, and pain management strategies can support the healing process, helping to alleviate symptoms and improve function.
What are the risks of leaving a herniated disc untreated?
Leaving a herniated disc untreated can lead to chronic pain and potentially more severe complications, such as permanent nerve damage. In cases where the spinal cord is compressed, untreated herniation can result in myelopathy, which may cause difficulty walking, coordination problems, and loss of bladder or bowel control.
How can ergonomic aids help with a herniated disc?
Ergonomic aids, such as supportive chairs, adjustable desks, and lumbar cushions, can help alleviate symptoms by promoting proper posture and reducing strain on the spine. These aids encourage a neutral spine position, which can prevent further injury and support recovery from a herniated disc.
Sources
- Barrow Neurological Institute. "Thoracic Disc Herniation Overview."
- Scoliosis Institute. "Understanding Thoracic Spine Conditions."
- Mayo Clinic. "Herniated Disc Symptoms and Causes."
- NewYork-Presbyterian. "Back Pain and Herniated Discs."
- Spine-health. "Non-Surgical Treatment for Thoracic Herniated Discs."
- Cleveland Clinic. "Differences Between Herniated and Bulging Discs."
- Miami Neuroscience Center. "Spinal Conditions and Treatments."