Back pain is a common ailment that affects millions of people worldwide, and one of the culprits often behind this discomfort is a herniated disc. This condition can significantly impact daily life, causing pain and limiting mobility. Understanding the nature of a herniated disc and how it heals is crucial for anyone dealing with this issue.
understanding the basics of a herniated disc
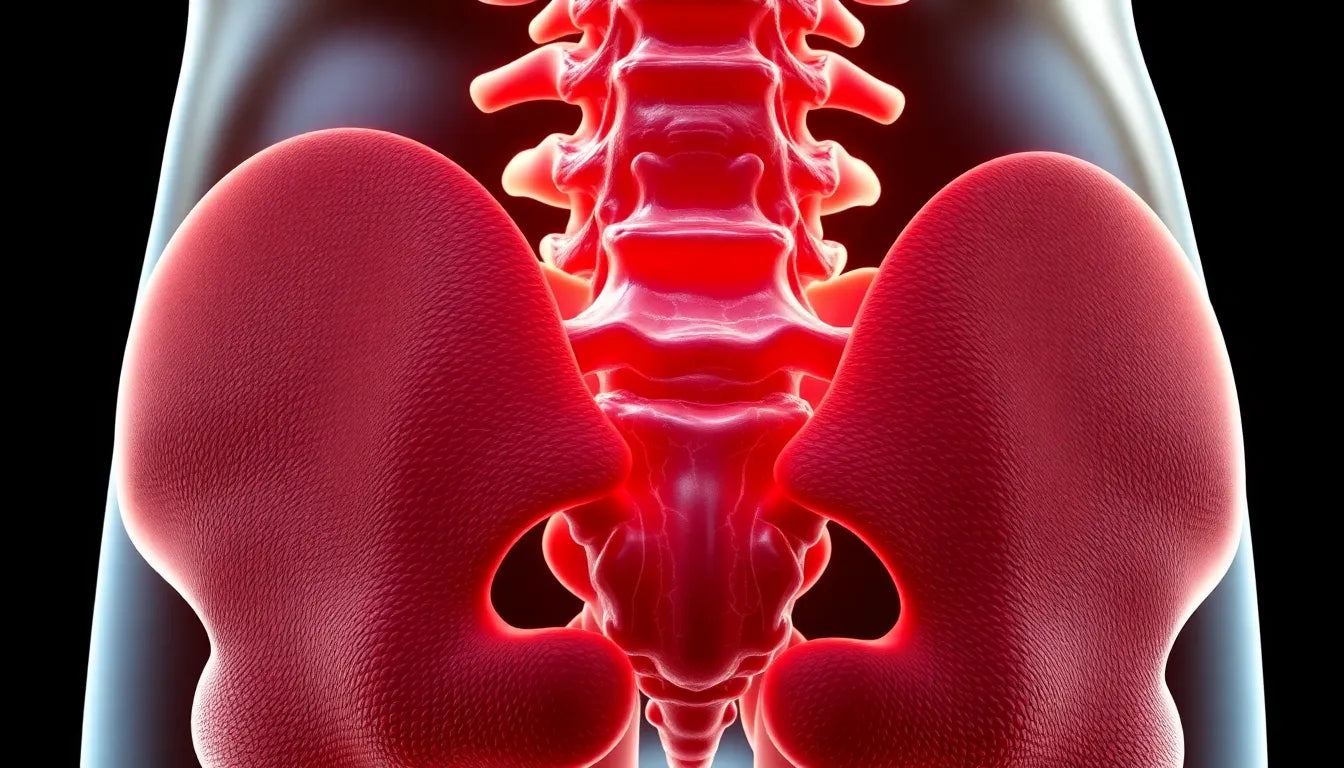
A herniated disc, sometimes referred to as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a tear in the tougher exterior. This can result from an injury, sudden strain, or the natural degeneration of the spine due to aging. The spine's discs act as cushions between the vertebrae, and when one is compromised, it can lead to significant discomfort.
The symptoms of a herniated disc can vary depending on the location and severity of the herniation. Common signs include back pain, numbness, and tingling sensations that may extend to the arms or legs. In severe cases, it can even affect muscle strength, making it difficult to perform everyday tasks.
importance of timely treatment
Addressing a herniated disc promptly is vital to managing pain and preventing further complications. The question that naturally arises for those suffering from this condition is: does a herniated disc heal? The answer isn't straightforward, as the healing process can vary significantly from person to person. However, understanding the potential for healing and the steps involved can empower individuals to take control of their recovery journey.
Timely intervention can help alleviate symptoms and improve quality of life. While some people might experience relief with conservative treatments, others may require more intensive interventions. Exploring the healing process and available treatments is essential for anyone seeking to regain their health and mobility.
In the following sections, we'll delve deeper into the phases of healing, factors influencing recovery, and the various treatment options available. Whether you're experiencing mild discomfort or severe pain, understanding the intricacies of herniated disc healing can provide clarity and hope.
healing timeline of a herniated disc
The healing journey of a herniated disc can be segmented into distinct phases, each contributing to the overall recovery process. Understanding these stages can provide insight into what to expect and how to manage symptoms effectively.
immediate phase
Immediately following the injury, the affected area is often marked by acute pain and inflammation. This phase can be the most painful, typically lasting between 2 to 8 weeks. During this time, the body's natural response is to protect the area and begin the healing process. Pain management is crucial, and patients may be advised to rest and use non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and alleviate discomfort.
subacute phase
As the initial inflammation begins to subside, the subacute phase commences. This period is characterized by a gradual reduction in pain and an improvement in mobility. Patients often start to regain some of their daily functions, although caution is still necessary to avoid re-injury. Physical therapy may be introduced to help strengthen the surrounding muscles and improve flexibility, facilitating a smoother transition to more active rehabilitation.
rehabilitation phase
The rehabilitation phase focuses on restoring full function and preventing future episodes. This stage involves a structured physical therapy regimen tailored to the individual's needs. Exercises aimed at strengthening the core, improving posture, and enhancing flexibility are integral components of this phase. Consistent participation in these exercises not only aids recovery but also plays a vital role in preventing recurrence by reinforcing the spine's support structures.
chronic phase
For some individuals, symptoms may persist beyond the typical recovery timeline, leading to a chronic phase. Long-term management strategies become essential for those experiencing ongoing discomfort. This may include continued physical therapy, lifestyle adjustments, and possibly more advanced interventions if conservative measures prove insufficient. Understanding that healing can be a prolonged process helps set realistic expectations and encourages adherence to treatment plans.
factors influencing the healing process
The healing of a herniated disc is influenced by several key factors that can vary widely among individuals. Recognizing these factors can help tailor treatment approaches and set realistic recovery goals.
severity of herniation
The size and location of the herniation play a significant role in determining the recovery timeline. Larger herniations or those pressing on nerve roots may require more intensive treatment and longer healing periods compared to smaller, less intrusive herniations.
patient's age and health
Age and overall health are critical determinants of the healing process. Younger individuals with robust health profiles often experience quicker recovery due to better regenerative capabilities. Conversely, older adults or those with underlying health conditions may face prolonged recovery times and may need more comprehensive management strategies.
lifestyle factors
Daily habits and lifestyle choices significantly impact the healing process. Maintaining a healthy weight reduces strain on the spine, while regular physical activity promotes circulation and muscle strength. Additionally, practicing good posture and ergonomics can prevent further stress on the discs and facilitate recovery.
treatment options for herniated discs
Effective management of a herniated disc often involves a combination of conservative and, in some cases, surgical interventions, depending on the severity and persistence of symptoms.
conservative treatments
Non-surgical approaches are typically the first line of treatment. These include the use of NSAIDs for pain relief, physical therapy to improve strength and flexibility, and chiropractic care to address spinal alignment issues. These methods aim to alleviate symptoms and promote natural healing.
surgical interventions
When conservative measures fail to provide adequate relief, or if there is significant nerve compression, surgical options may be considered. Procedures such as discectomy or laminectomy are performed to relieve pressure on the nerves and stabilize the spine. Surgery is usually reserved for cases where there is a clear indication of nerve damage or when pain severely impacts quality of life.
By understanding the phases of healing, factors influencing recovery, and available treatment options, individuals can make informed decisions about managing a herniated disc. This knowledge empowers patients to actively participate in their recovery journey, improving outcomes and enhancing quality of life.
complementary therapies and long-term management
Beyond conventional treatments, complementary therapies can play a supportive role in the healing of a herniated disc. Techniques such as acupuncture and massage therapy have gained popularity for their potential to alleviate pain and enhance well-being. Acupuncture, an ancient practice involving the insertion of thin needles into specific points on the body, is believed to stimulate natural healing processes and reduce inflammation. Similarly, massage therapy can help relax tight muscles, improve circulation, and promote a sense of relaxation, all of which contribute positively to recovery.
Long-term management of a herniated disc is essential for those who experience chronic symptoms. It involves a combination of lifestyle adjustments and ongoing treatment strategies aimed at maintaining spinal health and preventing future issues. Regular physical activity, tailored to individual capabilities, is vital for strengthening the muscles that support the spine. Engaging in low-impact exercises such as swimming, walking, or cycling can help maintain fitness without placing undue stress on the back.
Additionally, ergonomic practices in daily life, such as using supportive seating and practicing proper lifting techniques, are crucial in reducing strain on the spine. Weight management also plays a significant role, as excess weight can increase pressure on the spinal discs. By adopting these strategies, individuals can manage their condition effectively and reduce the likelihood of recurrence.
frequently asked questions
Will I ever be able to run again with a herniated disc?
Returning to running after a herniated disc is possible, but it requires careful management and a gradual approach. It is crucial to follow a rehabilitation program that strengthens the core and improves flexibility. Consulting with a healthcare professional to assess readiness and develop a personalized plan is advisable. Once cleared, start with low-impact activities, gradually increasing intensity as tolerated.
Is surgery always necessary for a herniated disc?
Surgery is not always necessary for a herniated disc. Many individuals find relief through conservative treatments such as physical therapy, medication, and lifestyle modifications. Surgery is typically considered when conservative measures fail to alleviate symptoms or if there is significant nerve compression leading to severe pain or neurological deficits. A thorough evaluation by a specialist can determine the most appropriate course of action.
How can I prevent a herniated disc from recurring?
Preventing recurrence involves adopting a proactive approach to spine health. This includes maintaining a regular exercise routine focused on strengthening the core, practicing good posture, and using ergonomic tools at work and home. Additionally, maintaining a healthy weight and avoiding activities that place excessive strain on the back are essential preventive measures.
What are the risks of not treating a herniated disc?
Neglecting treatment for a herniated disc can lead to chronic pain and potential complications such as nerve damage or muscle weakness. Untreated herniations may also cause permanent changes in sensation or movement. Early intervention and appropriate management can prevent these outcomes and improve quality of life.
How soon can I expect relief from symptoms?
Relief from symptoms can vary depending on the severity of the herniation and individual factors. Generally, pain may begin to subside within 2 to 8 weeks with appropriate treatment. However, full recovery can take several months. Adhering to a structured treatment plan and making necessary lifestyle adjustments can expedite recovery and enhance overall outcomes.