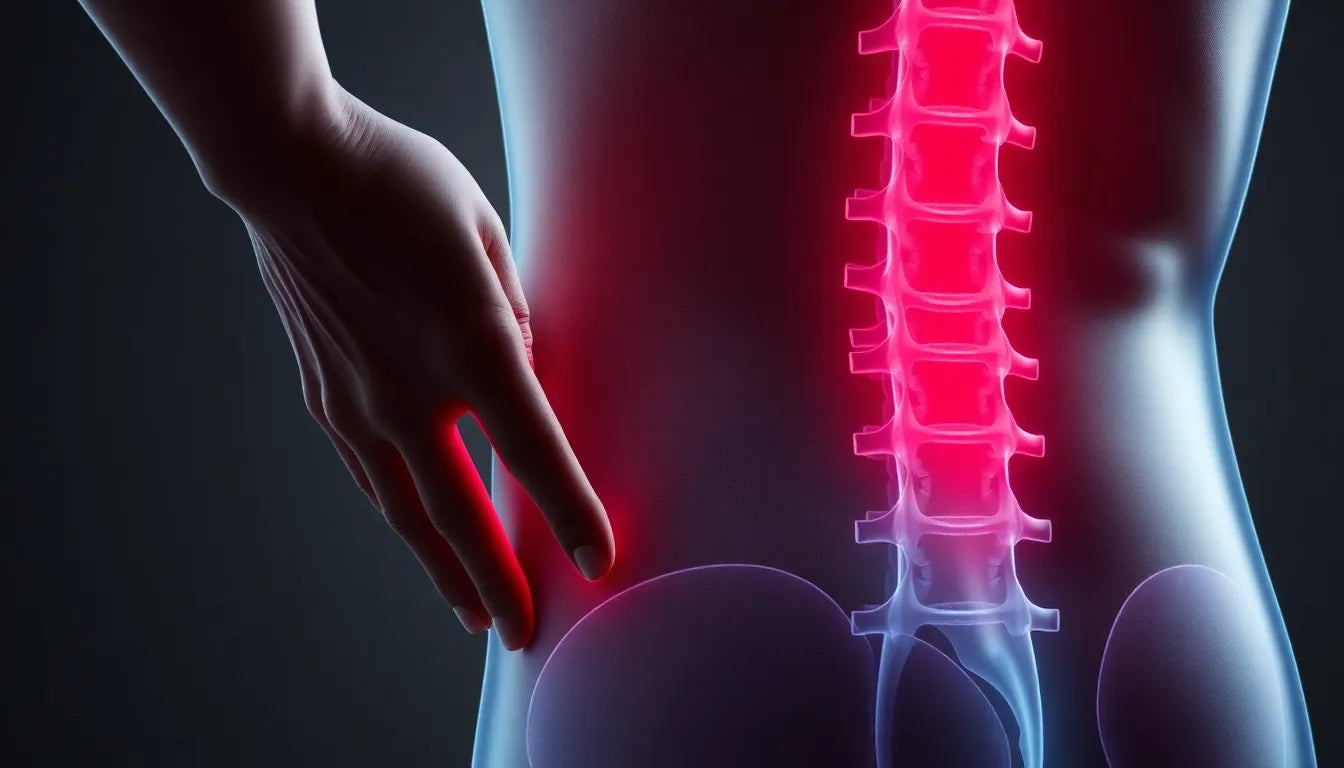
Dealing with a herniated disc in the lower back can be a daunting experience, yet understanding the condition and exploring non-surgical solutions can significantly ease the journey towards recovery. A herniated disc, often referred to as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a crack in the tougher exterior casing. This condition frequently affects the lumbar spine, the lower part of the back, and can lead to discomfort and disability.
Understanding herniated discs
The lumbar spine is particularly susceptible to herniated discs due to the significant weight and stress it bears. Common causes include heavy lifting, age-related degeneration, and sudden movements that put undue pressure on the spine. As we age, the spinal discs naturally lose some of their water content, making them less flexible and more prone to tearing or rupturing with even minor strains or twists.
Symptoms of a herniated disc in the lower back can vary, but often include persistent pain, numbness, tingling, and muscle weakness. These symptoms typically radiate from the lower back to the legs, a condition known as sciatica, which can severely impact mobility and quality of life.
The importance of non-surgical solutions
While the prospect of surgery might seem like a quick fix, non-surgical solutions are generally recommended as the first line of treatment for a herniated disc. This conservative approach is favored due to its less invasive nature, reduced risk of complications, and often effective results in managing symptoms.
Non-surgical methods focus on alleviating pain and improving function without the need for invasive procedures. They include a range of therapies such as physical therapy, exercise, medication, and lifestyle modifications, which not only target symptom relief but also address the underlying causes of the condition. By strengthening the muscles surrounding the spine and improving posture, these methods can help prevent future occurrences.
Moreover, opting for non-surgical solutions allows for a personalized treatment plan tailored to the individual's specific needs and lifestyle. This approach empowers patients to take an active role in their recovery, promoting long-term health and well-being.
In conclusion, understanding the nature of a herniated disc and exploring effective non-surgical solutions can pave the way for a successful recovery. By prioritizing conservative treatments, individuals can manage their symptoms and improve their quality of life without the need for invasive procedures. In the following sections, we will delve deeper into the various non-surgical options available and how they can be effectively utilized to heal a herniated disc in the lower back.
Exploring non-surgical treatment options
When dealing with a herniated disc in the lower back, non-surgical treatments play a pivotal role in alleviating pain and promoting recovery. These conservative approaches not only focus on symptom management but also aim to enhance overall spinal health, reducing the likelihood of future issues.
Rest and activity modification
One of the initial steps in managing a herniated disc involves rest and activity modification. It's crucial to strike a balance between rest and movement to prevent muscle stiffness and further complications. Limiting bed rest to just 1-2 days is often recommended to avoid weakening the muscles. Instead, gentle activity combined with frequent rest breaks can facilitate healing. Patients should avoid sitting for prolonged periods and incorporate light activities that do not strain the back.
The role of physical therapy and exercise
Physical therapy is a cornerstone of non-surgical treatment, focusing on exercises that strengthen the lower back and abdominal muscles. These exercises are designed to stabilize the spine, reducing pressure on the affected disc. Stretching exercises are equally important as they help maintain flexibility and alleviate tension. Incorporating aerobic exercises such as walking or stationary cycling can improve cardiovascular health and contribute to overall fitness, aiding in the recovery process.
Medication and pain relief strategies
For many individuals, medication is an effective means of managing pain and inflammation associated with a herniated disc. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are commonly prescribed to reduce pain and swelling. Additionally, hot and cold therapy can provide significant relief. Applying cold packs can help decrease inflammation, while heat pads can improve blood flow and relax tense muscles, promoting a sense of comfort.
Injections as a targeted approach
In cases where pain persists despite initial treatments, injections may be considered. Epidural steroid injections (ESIs) are a popular choice, offering both diagnostic and therapeutic benefits. With success rates ranging from 76-88%, ESIs can significantly reduce pain and inflammation. Another option, selective nerve root blocks (SNRBs), provides targeted pain relief with a success rate of about 75% for up to a year. These injections can be particularly beneficial for individuals seeking non-surgical solutions to manage their symptoms effectively.
Conclusion: embracing non-surgical solutions
Embracing non-surgical solutions for a herniated disc in the lower back can lead to significant improvements in pain management and overall quality of life. By prioritizing rest, engaging in targeted physical therapy, utilizing appropriate medications, and considering injections when necessary, individuals can effectively manage their condition without resorting to surgery. These conservative treatments not only address immediate symptoms but also focus on long-term spinal health, reducing the risk of future herniations.
In the next section, we will explore the circumstances under which surgical interventions may be considered, along with recovery expectations and when to seek further medical attention.
Surgical interventions for herniated discs
While non-surgical solutions remain the preferred approach for treating herniated discs, surgical interventions may become necessary when conservative treatments fail to provide adequate relief. Surgery is typically considered a last resort, reserved for cases where symptoms persist or worsen despite exhaustive non-invasive measures.
Common surgical procedures for herniated discs include discectomy, laminotomy, disc replacement surgery, and spinal fusion. A discectomy involves removing the portion of the disc that is pressing on the nerve, thereby relieving pressure and alleviating pain. Laminotomy, on the other hand, involves creating an opening in the lamina to access and remove the herniated material. In some cases, disc replacement surgery may be an option, where the damaged disc is replaced with an artificial one to maintain spinal mobility. Spinal fusion, often performed post-discectomy or laminotomy, stabilizes the spine by fusing two vertebrae together.
Recovery expectations and when to seek medical attention
Recovery from a herniated disc, when managed with conservative treatments, can vary significantly from person to person. Generally, individuals can expect a recovery timeline ranging from several weeks to a few months. Adhering to prescribed exercises and lifestyle modifications is crucial for optimizing recovery outcomes and preventing future issues. Patients should focus on maintaining a healthy weight, practicing good posture, and engaging in regular physical activity to support spinal health.
It is essential to seek medical attention if symptoms persist or worsen despite treatment. Warning signs such as severe weakness, loss of bladder or bowel control, or symptoms indicative of nerve damage require immediate medical evaluation. Early intervention can prevent further complications and aid in the recovery process.
Frequently asked questions
What are the first steps to take when diagnosed with a herniated disc?
Initial steps include resting for a short period and gradually reintroducing gentle activities. Consulting with a healthcare provider to develop a tailored treatment plan is crucial for effective management.
How long does it typically take to recover from a herniated disc without surgery?
Recovery can range from a few weeks to several months, depending on the severity of the condition and adherence to treatment protocols.
Are there lifestyle changes that can help prevent future herniated discs?
Yes, maintaining a healthy weight, practicing good posture, and engaging in regular exercise to strengthen core muscles can help prevent recurrence.
Is it possible for a herniated disc to heal on its own?
Many herniated discs can improve with time and conservative treatment, as the body absorbs the herniated material and inflammation decreases.
What role does diet play in managing a herniated disc?
A balanced diet rich in anti-inflammatory foods can support overall health and aid in the healing process.