Imagine waking up one morning, ready to tackle the day, only to be halted by a sharp, radiating pain in your lower back that shoots down your leg with every step. This unexpected scenario is a reality for many who struggle with a herniated disc, a condition that can significantly disrupt daily life. Understanding the early signs and symptoms is crucial in preventing further complications and maintaining a good quality of life.
Understanding herniated discs
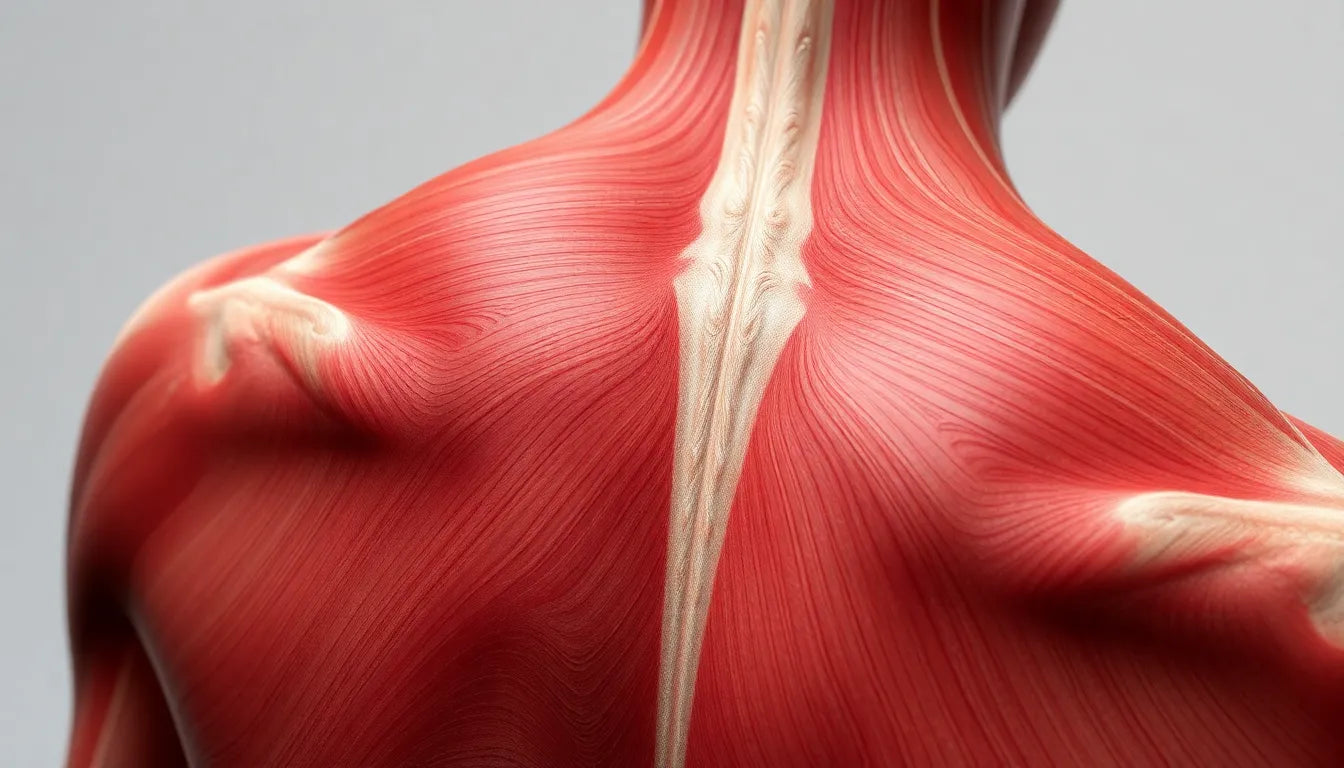
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a tear in its tougher outer layer. This can happen anywhere along the spine, but it most commonly affects the lower back (lumbar spine) or neck (cervical spine). The pressure exerted by the herniated material on nearby nerves can cause a range of symptoms, from mild discomfort to debilitating pain.
Herniated discs are surprisingly common, affecting individuals across various age groups and lifestyles. While they are often associated with aging, due to the natural wear and tear on spinal discs, younger individuals can also experience this condition, particularly if they engage in activities that put excessive strain on the back.
The importance of early detection
Recognizing the signs of a herniated disc early on is essential for preventing long-term damage and ensuring effective management of the condition. Early detection allows for timely intervention, which can significantly reduce the risk of chronic pain and improve overall outcomes. Identifying symptoms such as radiating pain, numbness, or muscle weakness can prompt individuals to seek medical advice sooner rather than later.
This blog post aims to guide you through the process of identifying the symptoms of a herniated disc, understanding the diagnostic procedures involved, and knowing when to seek professional medical help. By being informed, you can take proactive steps to address the issue before it escalates, ensuring that a herniated disc doesn't disrupt your life more than necessary.
Recognizing common symptoms of a herniated disc
Understanding the symptoms of a herniated disc is crucial for early intervention and effective management. The condition can manifest in various ways, depending on the location of the herniation and the nerves affected. Here are some of the most common symptoms to watch for:
Radiating pain
One of the hallmark signs of a herniated disc is radiating pain. This pain often starts in the back and travels to other parts of the body, depending on the location of the herniation:
- Lumbar herniation: Pain may radiate from the lower back to the buttocks, legs, calves, and even feet.
- Cervical herniation: Pain can extend from the neck into the shoulders and arms.
This pain is often described as sharp or burning and can significantly impact daily activities.
Numbness and tingling
Another common symptom is numbness or tingling in areas served by the affected nerves. This sensation can be unsettling and may affect your ability to perform routine tasks.
Muscle weakness
Muscle weakness is a critical symptom that can arise from a herniated disc. It can affect motor skills, making it challenging to grip or lift objects. This weakness typically corresponds to the nerve root affected by the herniation.
Unilateral symptoms
Interestingly, symptoms of a herniated disc often appear on only one side of the body, depending on which nerve is compressed. This unilateral presentation can help in pinpointing the affected area.
Aggravating factors
Certain activities can exacerbate the pain associated with a herniated disc. Movement, sitting for extended periods, sneezing, or coughing can all intensify the discomfort, making it important to identify and avoid these triggers when possible.
Understanding asymptomatic cases
It's important to note that not everyone with a herniated disc experiences symptoms. Many people may have a herniated disc discovered incidentally during imaging for unrelated issues. This asymptomatic nature underscores the importance of regular check-ups, especially if you're at risk due to lifestyle or age.
Recognizing emergency symptoms
While many herniated discs can be managed conservatively, certain symptoms require immediate medical attention. These include:
- Severe pain or weakness that disrupts daily activities.
- Numbness in the genital or rectal area.
- Loss of bladder or bowel control.
- New symptoms in individuals with a history of metastatic cancer.
If you experience any of these symptoms, it is crucial to seek medical help without delay, as they may indicate a more serious condition requiring urgent intervention.
Diagnosing a herniated disc
Diagnosing a herniated disc typically involves a combination of physical examination, medical history review, and imaging techniques:
Physical examination
Your healthcare provider will assess your pain levels, muscle strength, reflexes, and sensation to determine the extent of nerve involvement and the likely location of the herniation.
Medical history review
A thorough review of your medical history helps correlate symptoms with potential causes and risk factors, providing valuable context for diagnosis.
Imaging techniques
Imaging is often used to confirm a diagnosis and assess the extent of the herniation:
| Technique | Description |
|---|---|
| MRI | The gold standard for visualizing herniated discs and nerve involvement. |
| CT Scan | Provides a detailed view of bony structures, especially useful if MRI is not available. |
| X-rays | Used to rule out other causes, though they do not show herniated discs themselves. |
| Myelogram | A dye test for visualizing the spinal cord and nerve roots, usually followed by a CT scan. |
Nerve function tests
Electromyogram (EMG) and nerve conduction studies are used to assess the function of nerves and muscles, helping pinpoint nerve damage or compression.
By understanding these symptoms and diagnostic processes, you can take proactive steps to manage a herniated disc effectively. Early detection and appropriate medical intervention are key to preventing further complications and maintaining a good quality of life.
Self-management and medical treatment for herniated discs
Once a herniated disc is diagnosed, the focus often shifts to managing the symptoms and preventing further complications. Initial treatment usually involves non-surgical approaches:
- Over-the-counter pain relievers: Medications such as ibuprofen or acetaminophen can help reduce pain and inflammation.
- Physical therapy: A structured exercise program can strengthen the muscles around the spine, improve flexibility, and reduce pressure on the affected nerves.
- Activity modification: Adjusting daily activities to avoid movements that exacerbate symptoms is crucial for recovery. This may include avoiding heavy lifting or prolonged sitting.
In most cases, these conservative treatments are successful, and surgery is not required. However, if symptoms persist or worsen, a healthcare provider may recommend more invasive procedures.
Conclusion: The importance of early recognition
Identifying the signs of a herniated disc early and seeking appropriate medical care can significantly improve outcomes and quality of life. By understanding the symptoms and diagnostic processes, individuals can take proactive steps to manage their condition effectively. Additionally, ergonomic aids, such as supportive chairs or cushions, can play a role in maintaining spinal health and alleviating discomfort. However, it is essential to consult healthcare professionals before making significant lifestyle or treatment changes.
Frequently Asked Questions
What are the early signs of a herniated disc?
Early signs include radiating pain, numbness, tingling, and muscle weakness, often affecting one side of the body. These symptoms can vary based on the location of the herniation.
When should I see a doctor?
It is advisable to seek medical advice if you experience persistent pain, numbness, or weakness. Immediate medical attention is necessary for severe symptoms, such as loss of bladder or bowel control or numbness in the genital area.
Can a herniated disc heal on its own?
Many herniated discs improve over time with conservative treatment. Factors such as age, overall health, and adherence to treatment plans can influence recovery. However, medical evaluation is essential to guide appropriate management.
What lifestyle changes can help manage symptoms?
Incorporating ergonomic adjustments, like using supportive chairs and maintaining proper posture, can alleviate discomfort. Regular low-impact exercises, such as walking or swimming, can also help maintain spinal health.
Is surgery always necessary for a herniated disc?
Surgery is often a last resort, reserved for cases where conservative treatments fail to relieve symptoms or when severe symptoms, such as neurological deficits, are present. Most individuals manage successfully with non-surgical treatments.
Sources
- Mayo Clinic. "Herniated Disk: Symptoms and Causes."
- Cleveland Clinic. "Herniated Disc: Diagnosis and Tests."
- WebMD. "Herniated Disc: Symptoms and Treatment."
- Penn Medicine. "Herniated Disc: Diagnosis and Treatment Options."
- Weill Cornell Medicine. "Understanding Herniated Discs: Diagnostic Tools."
- NYU Langone Health. "Herniated Disc in Adults: Diagnosis and Treatment."