Understanding the signs of a herniated disc is crucial for maintaining spinal health and ensuring timely intervention. A herniated disc, also known as a slipped or ruptured disc, occurs when the soft, gel-like center of a spinal disc pushes through a tear in its tougher outer layer. This condition can lead to significant discomfort and mobility issues, making early detection vital in preventing further complications.
Understanding herniated discs
A herniated disc can affect anyone, but it is most prevalent among individuals aged 30 to 50. This condition often arises from wear and tear over time, known as disc degeneration, or from sudden injury. The spine's discs act as cushions between vertebrae, absorbing shock and allowing for flexibility. When one of these discs herniates, the leaked material can irritate nearby nerves, leading to pain, numbness, or weakness in the limbs.
Early detection of a herniated disc is essential. Recognizing the symptoms can guide you to seek appropriate treatment and avoid potential complications such as chronic pain or permanent nerve damage. While some people experience severe symptoms, others may have a herniated disc without realizing it, as they remain asymptomatic. This variability underscores the importance of understanding the signs and seeking a professional evaluation if you suspect an issue.
Why knowing the signs matters
Identifying the symptoms of a herniated disc is critical because the impact on daily life can be significant. Pain from a herniated disc is often described as sharp or burning, and it may radiate to the arms or legs, depending on the location of the affected disc. This pain can extend to the buttocks, thighs, calves, or feet, potentially leading to decreased mobility and a reduced quality of life.
Moreover, some individuals may experience numbness, tingling, or muscle weakness in areas served by the affected nerves. These symptoms can complicate self-diagnosis, as they might be attributed to other conditions. Therefore, professional evaluation is crucial. A healthcare provider can perform a thorough assessment, including a medical history review and physical examination, to determine the cause of your symptoms and recommend an appropriate course of action.
In conclusion, understanding how to know if you have a herniated disc is key to managing your spinal health effectively. By recognizing the symptoms and seeking timely medical advice, you can prevent the condition from worsening and maintain a better quality of life. Stay informed, be proactive, and consult a healthcare professional if you suspect a herniated disc. Your spine will thank you for it.
Common symptoms of a herniated disc
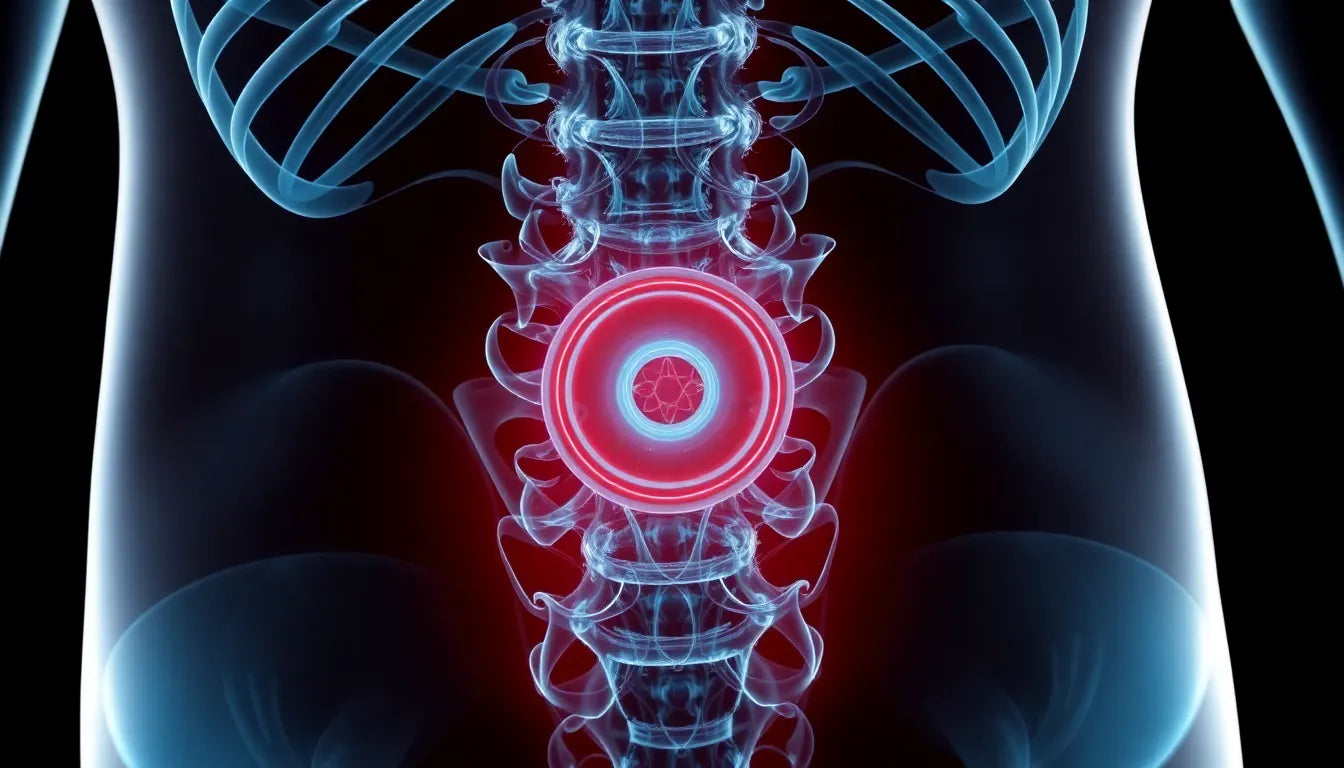
Recognizing the symptoms of a herniated disc is vital for determining whether you might be affected by this condition. The most prevalent symptom is radiating pain, which can manifest as sharp or shooting sensations. This pain often extends to the arms or legs, depending on the location of the herniated disc. For example, if the herniation occurs in the lower back, you might experience discomfort in the buttocks, thighs, calves, or even feet. This kind of pain can significantly impact your daily activities and overall quality of life.
Another common symptom is numbness and tingling. These sensory changes occur because the herniated disc can compress nearby nerves, leading to altered sensations in the areas served by those nerves. You might feel tingling or a pins-and-needles sensation in your arms or legs, which can be unsettling and disruptive.
Muscle weakness is also a potential indicator of a herniated disc. The compression of nerves can affect the muscles they control, leading to weakness. This weakness can impact your physical capabilities, making it challenging to perform everyday tasks and activities. You might notice difficulty in maintaining balance or coordination, which can further affect your lifestyle.
Diagnosis process for herniated discs
Getting a professional diagnosis is crucial if you suspect a herniated disc. The process typically begins with an initial medical evaluation, where a healthcare provider will take your medical history and conduct a physical examination. During this assessment, the doctor will evaluate your pain patterns, check for sensory changes such as numbness or tingling, and test your reflexes, muscle strength, and gait. Specific physical tests, like the straight leg raise, may be used to determine nerve involvement and pinpoint the affected areas.
If your symptoms persist or are severe, imaging and advanced diagnostics might be necessary. Magnetic resonance imaging (MRI) is considered the gold standard for identifying herniated discs and any associated nerve compression. It provides detailed images of the spinal structures, helping doctors confirm the diagnosis and plan appropriate treatment. In some cases, if MRI results are inconclusive or unavailable, computed tomography (CT) scans or myelograms may be used to get a clearer picture of the spine.
In situations where the diagnosis remains unclear, nerve conduction studies or electromyography (EMG) might be employed. These tests assess the electrical activity of muscles and nerves, helping to pinpoint nerve damage and determine its severity. Although routine X-rays are not effective in detecting herniated discs, they can help rule out other spine problems that might be causing your symptoms.
Conclusion
Understanding how to know if you have a herniated disc involves recognizing the common symptoms and seeking professional evaluation. Radiating pain, numbness, tingling, and muscle weakness are key indicators that should not be ignored. Early diagnosis and intervention are crucial for managing symptoms and preventing further complications. If you experience any of these symptoms, especially if they persist or worsen, consult a healthcare professional for a thorough assessment. By staying informed and proactive, you can take control of your spinal health and maintain a better quality of life.
Emergency symptoms and when to seek immediate care
While many cases of herniated discs can be managed with non-surgical treatments, certain symptoms require urgent medical attention. These include bowel or bladder dysfunction, progressive weakness, and severe, incapacitating pain. These symptoms may indicate a more serious condition, such as cauda equina syndrome, which requires immediate surgical intervention to prevent permanent damage.
If you experience any of these red flags, it is crucial to seek emergency care without delay. Early intervention can significantly improve outcomes and prevent further complications. Remember, your health and well-being are paramount, and addressing these symptoms promptly can make a substantial difference.
Frequently Asked Questions
What causes a herniated disc?
A herniated disc can result from several factors, including aging, injury, and repetitive strain. As we age, our spinal discs naturally lose some of their water content, making them less flexible and more prone to tearing or rupturing with even minor strain or twist. Injuries from lifting heavy objects improperly or sudden trauma can also cause a disc to herniate.
Can a herniated disc heal on its own?
In some cases, a herniated disc can heal on its own over time with rest and appropriate care. The body may reabsorb the herniated material, reducing pressure on the nerves and alleviating symptoms. Factors such as the severity of the herniation, the individual's overall health, and adherence to treatment recommendations can influence recovery. Consulting a healthcare professional is essential to determine the best course of action.
What are the treatment options for a herniated disc?
Treatment for a herniated disc varies depending on the severity of symptoms. Non-surgical options include physical therapy, medications such as anti-inflammatory drugs or muscle relaxants, and lifestyle modifications. In more severe cases, surgical interventions like microdiscectomy or spinal fusion may be considered to relieve nerve pressure and stabilize the spine.
How can I prevent a herniated disc?
Preventing a herniated disc involves maintaining good spinal health through proper body mechanics and lifestyle choices. Practicing correct lifting techniques, engaging in regular exercise to strengthen core muscles, and making ergonomic adjustments in the workplace can help reduce the risk. Additionally, maintaining a healthy weight and avoiding smoking can contribute to overall spine health.
When should I see a doctor for back pain?
It is advisable to see a doctor if you experience persistent back pain, especially if it is accompanied by numbness, tingling, or muscle weakness. If your symptoms worsen or do not improve with self-care measures, a professional evaluation is necessary. Early diagnosis and treatment can prevent further complications and improve your quality of life.
Understanding the signs of a herniated disc and knowing when to seek medical advice are crucial steps in managing your spinal health. By staying informed and proactive, you can take control of your health and ensure the best possible outcomes.
Sources
- Mayo Clinic. "Herniated Disk: Symptoms and Causes."
- Cleveland Clinic. "Herniated Disk: Symptoms, Causes, and Treatment."
- WebMD. "Herniated Disc: Overview and Symptoms."
- Spine-health. "Herniated Disc: Diagnosis and Treatment Options."
- Penn Medicine. "Herniated Disc: Causes and Diagnosis."
- University of Maryland Medical Center. "Herniated Disc: Patient Guide."