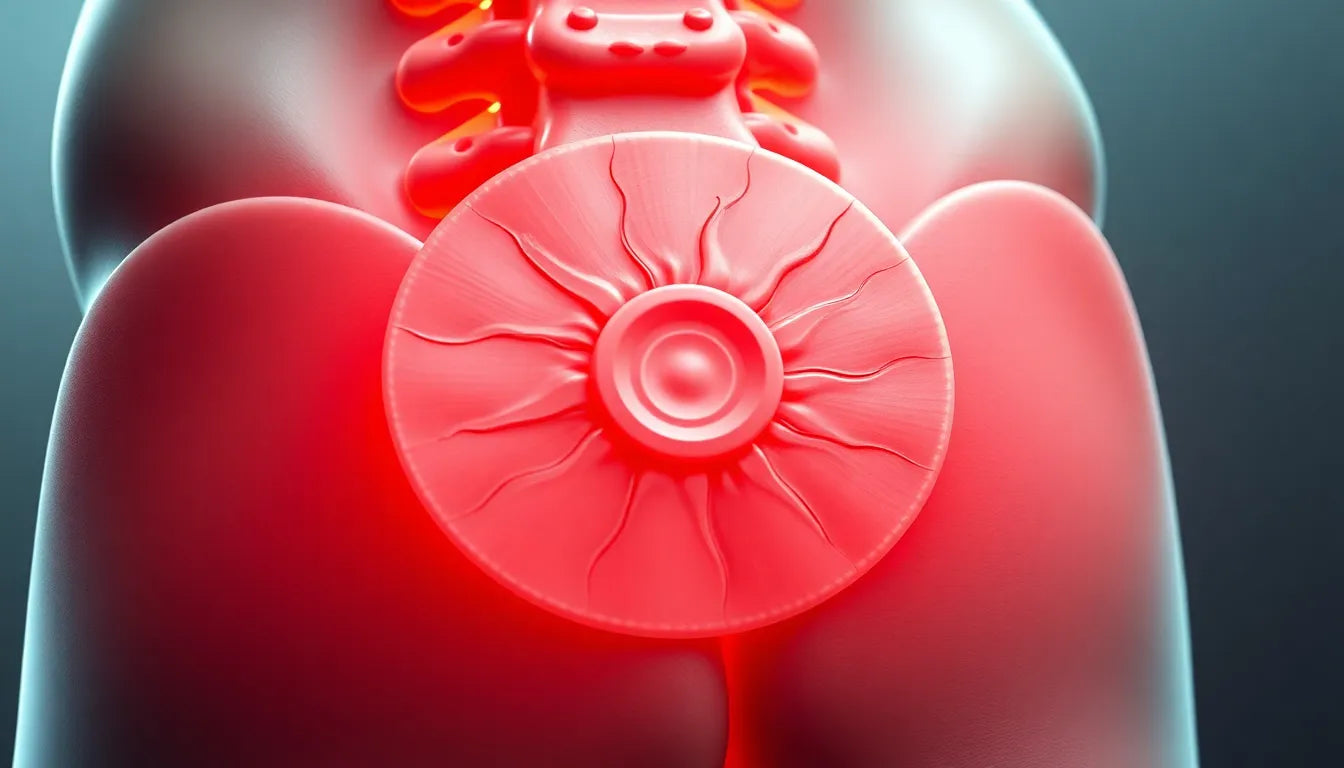
Herniated discs are a common spinal condition that can lead to a variety of symptoms, one of the most notable being sensory disturbances. A herniated disc occurs when the nucleus of a spinal disc pushes through a tear in its outer layer, often resulting in nerve root compression. This compression can lead to sensory disturbances such as numbness, tingling, and changes in skin sensation, which are frequently experienced by individuals with this condition.
Understanding sensory disturbances in herniated discs
Sensory disturbances are a significant symptom of herniated discs, affecting a large number of individuals who suffer from this condition. These disturbances can manifest as numbness, tingling sensations, or even a complete change in skin sensation, depending on the severity and location of the herniation. Understanding these symptoms is crucial, as they can indicate the specific area of the spine affected by the herniated disc. For instance, herniations in the lumbar spine often lead to sensory loss in areas such as the thigh, calf, or foot, depending on the specific nerve root involved.
Impact on daily life and the importance of early recognition
The presence of sensory disturbances due to a herniated disc can significantly impact an individual's daily life. These symptoms can affect mobility, limit physical activities, and reduce overall quality of life. Tasks that were once simple can become challenging, and the discomfort from these disturbances can lead to frustration and stress. Early recognition and management of these sensory disturbances are essential to prevent further complications and to improve the patient's quality of life. Addressing these symptoms promptly can help individuals maintain their daily routines and avoid the progression of symptoms.
Purpose of understanding herniated disc sensory disturbances
The primary purpose of this post is to educate readers about the causes, symptoms, and management strategies for sensory disturbances associated with herniated discs. By understanding the nature of these symptoms and their implications, individuals can better recognize the signs and seek appropriate medical attention. This knowledge can empower patients to take control of their health, make informed decisions about their treatment options, and ultimately improve their overall well-being. Through this post, we aim to provide valuable insights into the complexities of sensory disturbances in herniated discs and offer guidance on how to manage them effectively.
Causes and mechanism of sensory disturbances in herniated discs
Understanding the causes and mechanisms behind sensory disturbances in herniated discs is crucial for effective management. Sensory disturbances primarily arise due to nerve root compression, which occurs when the protruding disc material exerts pressure on the spinal nerve roots. These nerve roots are responsible for transmitting sensory information from various parts of the body to the brain. When compressed, they can lead to altered or diminished sensation, such as numbness and tingling.
The specific sensory symptoms experienced depend largely on the location of the herniation along the spine. For instance, herniations in the lumbar region often lead to sensory disturbances in the lower extremities, while those in the thoracic region can affect areas around the chest and upper back. This relationship between the herniation's location and the resulting sensory symptoms is essential for accurate diagnosis and targeted treatment.
Detailed mapping of sensory loss by spinal nerve
A detailed understanding of sensory loss patterns can help in identifying the affected spinal nerve roots. In the lumbar spine, specific nerve roots correspond to distinct areas of sensory disturbance:
- L1: Sensory loss typically occurs in the inguinal region.
- L2-L4: These nerve roots are associated with sensory deficits in the anterior thigh and medial lower leg.
- L5: Disturbances often present on the lateral calf, dorsum of the foot, and the web space between the first and second toe.
- S1: Sensory loss is commonly found on the posterior calf and lateral or plantar foot.
- Severe cases (S2-S4): These can lead to sensory changes in the buttock, perineal, and perianal regions, sometimes accompanied by incontinence.
In the thoracic spine, herniations can cause mid-back pain and sensory disturbances that wrap around the chest. Additionally, these herniations may lead to progressive numbness or weakness in the lower extremities, complicating mobility and daily activities.
Associated symptoms and diagnosis
Sensory disturbances are rarely isolated symptoms; they often occur alongside other manifestations such as pain and motor deficits, including muscle weakness and changes in reflexes. The presence of these additional symptoms can complicate the clinical picture, necessitating a comprehensive diagnostic approach.
The diagnostic process for sensory disturbances associated with herniated discs typically involves a thorough neurological examination. This examination focuses on identifying patterns of sensory loss, assessing reflexes, and evaluating muscle strength. Imaging techniques, such as MRI or CT scans, play a crucial role in visualizing the herniated disc and the extent of nerve root compression. Additionally, nerve conduction studies may be employed to assess the functional impact on nerve signaling.
By accurately diagnosing the affected nerve roots and understanding the extent of sensory disturbances, healthcare providers can develop a tailored treatment plan. This plan aims to alleviate symptoms, restore function, and improve the patient's overall quality of life.
Management and treatment options for sensory disturbances
Addressing sensory disturbances in herniated discs requires a multi-faceted approach tailored to the severity and progression of symptoms. For many patients, conservative management is the first line of treatment. This includes rest, physical therapy, and the use of non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and alleviate pain. Additionally, nerve pain medications such as gabapentin or duloxetine can be prescribed to specifically target neuropathic pain, providing further relief from sensory disturbances.
For individuals experiencing persistent symptoms, interventional options such as epidural steroid injections and selective nerve root blocks may be considered. These procedures aim to reduce inflammation around the affected nerve roots, thereby decreasing sensory disturbances and improving overall function.
In cases where conservative and interventional treatments do not yield sufficient improvement, surgical treatment may be necessary. Surgical options, such as discectomy, focus on relieving nerve compression by removing or repairing the herniated disc material. Both endoscopic and traditional surgical approaches can be effective, with the choice depending on the specific clinical scenario and patient preference.
In addition to these primary treatments, adjunct therapies like electrotherapy and functional electrical stimulation can be beneficial. These therapies are particularly useful in rehabilitation settings, aiding in sensory-motor recovery and enhancing overall outcomes.
Practical tips for managing sensory disturbances
Incorporating practical strategies into daily life can significantly help manage sensory disturbances. Ergonomic aids, such as supportive chairs and cushions, can reduce further nerve compression and promote optimal body positioning. Additionally, being mindful of posture and avoiding prolonged periods in positions that exacerbate symptoms can prevent worsening of sensory disturbances.
Engaging in regular, gentle physical activity can also be beneficial. Exercises that strengthen core muscles and improve flexibility may reduce strain on the spine, thereby alleviating pressure on the affected nerve roots. Consulting with a physical therapist can provide personalized exercise recommendations and guidance on safe activity levels.
Frequently Asked Questions
What are the common sensory disturbances in herniated discs?
The most common sensory disturbances associated with herniated discs include numbness, tingling, and changes in skin sensation. These symptoms occur due to nerve root compression and vary depending on the location of the herniation along the spine.
How are sensory disturbances diagnosed?
Diagnosis of sensory disturbances involves a comprehensive neurological examination focusing on sensory loss patterns, reflexes, and muscle strength. Imaging techniques such as MRI or CT scans help visualize the herniated disc and assess nerve root compression. Nerve conduction studies may also be used to evaluate nerve function.
What are the treatment options for sensory disturbances?
Treatment options for sensory disturbances range from conservative management, including rest and medications, to interventional procedures like epidural steroid injections. Surgical treatment may be considered for severe cases. Adjunct therapies such as electrotherapy can also support recovery.
Can sensory disturbances be prevented?
While not all sensory disturbances can be prevented, maintaining good posture, using ergonomic aids, and engaging in regular physical activity can help manage and reduce symptoms. Early recognition and treatment are crucial in preventing further complications.
Sources
- Physio-Pedia. "Disc Herniation."
- Barrow Neurological Institute. "Herniated Disc - Symptoms, Diagnosis, Treatment."
- Mayo Clinic. "Herniated Disk - Symptoms and Causes."
- STIWELL/Med-El. "Electrotherapy for Spinal Cord Injury Rehabilitation."
- Sciatica.com. "Herniated Disc Pain Management."
- OrthoInfo (AAOS). "Lumbar Disc Herniation."