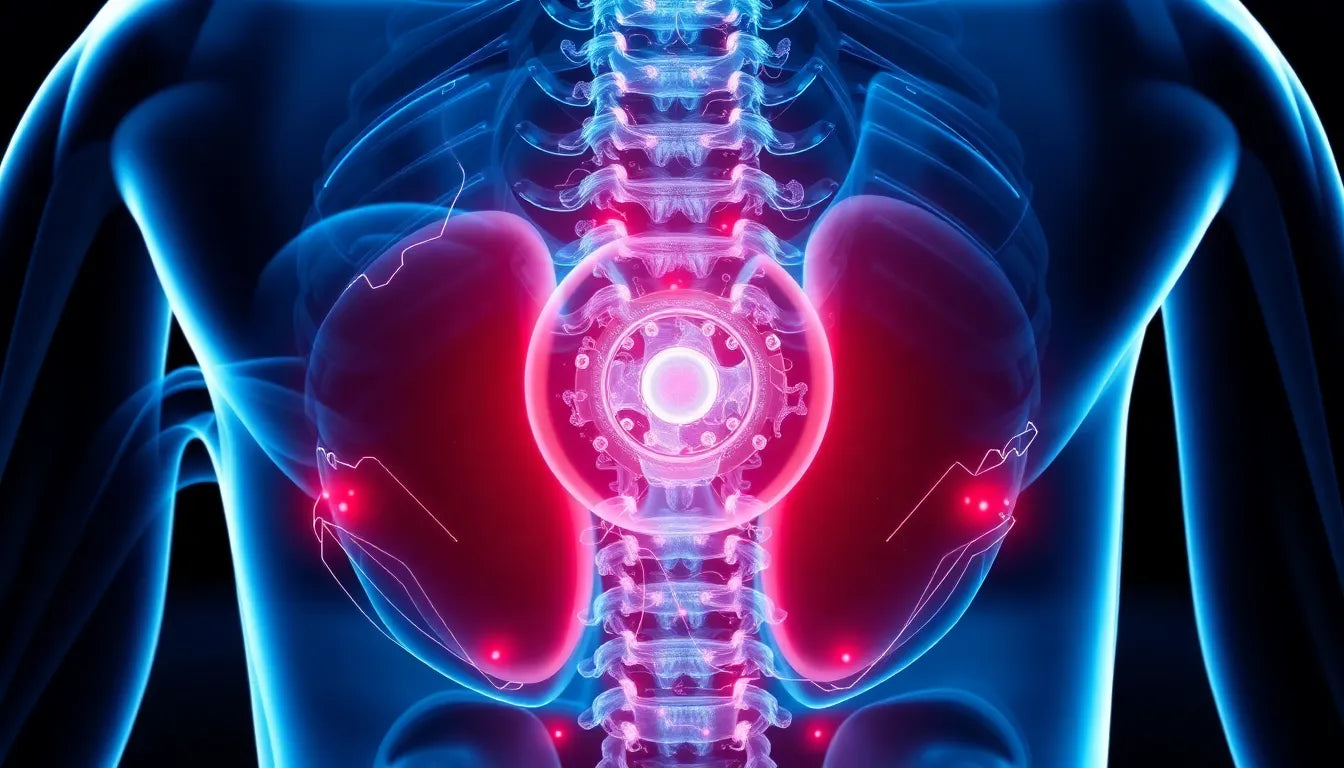
Spondylosis is a term that often emerges in discussions about back health, yet its meaning can sometimes be elusive. Essentially, spondylosis refers to a degenerative condition of the spine, more commonly known as spinal osteoarthritis. This condition represents the natural "wear and tear" process that our spines undergo as we age. Affecting millions of people worldwide, spondylosis is a prevalent age-related condition that can have significant implications for daily life and mobility.
Understanding the prevalence of spondylosis
As we age, our bodies inevitably undergo various changes, and the spine is no exception. Spondylosis is a common manifestation of these changes, characterized by the degeneration of the intervertebral discs and facet joints. This degenerative process is primarily due to aging, but it can also be accelerated by mechanical stress or trauma. The prevalence of spondylosis increases with age, making it a condition that affects a large portion of the population, especially those over the age of 50.
The importance of understanding spondylosis
Understanding spondylosis is crucial for managing its symptoms and improving quality of life. Many people experience confusion when it comes to spinal conditions, often mixing up terms like spondylosis, spondylitis, and spondylolisthesis. Each of these conditions has distinct characteristics and implications, so distinguishing between them is important for proper diagnosis and treatment.
Recognizing spondylosis as a degenerative condition rather than an inflammatory one, like spondylitis, helps in understanding the nature of the symptoms and the appropriate management strategies. While spondylosis itself cannot be reversed, understanding its mechanics can lead to better symptom management and potentially slow its progression through lifestyle adjustments and targeted therapies.
The implications of spondylosis extend beyond mere physical discomfort. As it affects the spine's integrity, it can lead to reduced mobility and flexibility, impacting daily activities and overall quality of life. By gaining a comprehensive understanding of spondylosis, individuals can take proactive steps to manage their symptoms, maintain mobility, and improve their quality of life despite the challenges posed by this condition.
In the following sections, we will delve deeper into the specifics of spondylosis, examining its causes, the areas of the spine it affects, and the symptoms it presents. By shedding light on these aspects, we aim to provide a clearer picture of what spondylosis entails and how it can be effectively managed.
delving into the causes and definition of spondylosis
Spondylosis is fundamentally understood as a degenerative process affecting the intervertebral discs and facet joints, often attributed to the natural aging process. As we age, the discs that act as cushions between the vertebrae begin to lose hydration and elasticity, leading to a gradual breakdown. This degeneration can result in the loss of disc height, which subsequently increases mechanical stress on the facet joints. In some cases, trauma or repetitive mechanical stress can accelerate this degenerative process, exacerbating the condition.
Mechanical stress plays a significant role in the progression of spondylosis. Activities that involve repetitive bending, twisting, or heavy lifting can increase the wear and tear on the spine. Over time, this can lead to the formation of bone spurs, or osteophytes, which are bony projections that develop along the edges of bones. These spurs can contribute to the narrowing of the spinal canal or the spaces where nerves exit the spine, potentially leading to nerve compression and associated symptoms.
areas of the spine affected by spondylosis
Spondylosis can affect various regions of the spine, each presenting unique challenges and symptoms. The most common areas affected are the cervical (neck) and lumbar (lower back) regions, although the thoracic (mid-back) region can also be involved.
cervical spondylosis
Cervical spondylosis refers to the degenerative changes occurring in the neck region. This form of spondylosis can lead to symptoms such as neck pain, stiffness, and in some cases, herniated discs that may compress nearby nerves. This nerve compression can result in symptoms radiating down the arms, such as tingling, numbness, or weakness.
thoracic spondylosis
While less common than cervical or lumbar spondylosis, thoracic spondylosis affects the mid-back region. Due to the rib cage's support, this area of the spine is less mobile and experiences less mechanical stress, making degenerative changes here less frequent. However, when thoracic spondylosis does occur, it can lead to mid-back pain and stiffness.
lumbar spondylosis
Lumbar spondylosis is the degeneration of the lower back region, often due to significant mechanical stress from activities like lifting or prolonged sitting. This type of spondylosis can be associated with conditions like spinal stenosis, where the spinal canal narrows, potentially compressing nerves and leading to symptoms like lower back pain, leg pain, and difficulty walking.
symptoms and diagnostic methods
The symptoms of spondylosis can vary widely, ranging from mild discomfort to significant pain and reduced mobility. Common symptoms include chronic pain, stiffness, and a decrease in flexibility. It's important to note that the severity of symptoms does not always correlate with the degree of degeneration visible on imaging studies. Some individuals may have significant degenerative changes visible on X-rays or MRIs but experience minimal symptoms, while others may have severe symptoms with only mild imaging findings.
Diagnosing spondylosis typically involves imaging techniques such as X-rays, MRI (Magnetic Resonance Imaging), and CT (Computed Tomography) scans. X-rays can reveal changes in bone structure, such as bone spurs or disc space narrowing. MRI and CT scans provide detailed images of both bone and soft tissues, helping to assess the extent of disc degeneration and any potential nerve compression.
Understanding the specific causes, affected areas, and symptoms of spondylosis is crucial for developing effective management strategies. By identifying the particular region of the spine affected and the severity of the condition, healthcare providers can tailor treatment plans to address individual needs and improve quality of life.
Impact of lifestyle and aging on spondylosis
Lifestyle choices and the natural aging process both play significant roles in the development and progression of spondylosis. As we age, the spinal discs lose hydration and elasticity, contributing to the degenerative changes associated with spondylosis. However, lifestyle factors such as posture, physical activity, and ergonomics can influence how these changes manifest and progress.
Maintaining good posture is crucial for minimizing mechanical stress on the spine. Poor posture can exacerbate the wear and tear on spinal structures, potentially accelerating degeneration. Regular physical activity, particularly exercises that strengthen the core and improve flexibility, can help support the spine and reduce the impact of spondylosis. Additionally, ergonomic adjustments in daily life, such as using supportive chairs and maintaining proper desk setups, can help manage symptoms and slow the condition's progression.
Clarifying spinal condition terminology
Understanding the differences between spondylosis and other spinal conditions is essential for accurate diagnosis and treatment. Spondylosis is often confused with similar-sounding conditions, but each has distinct characteristics:
- Spondylitis: This refers to an inflammatory condition of the spine, often associated with autoimmune disorders. Unlike spondylosis, which is degenerative, spondylitis involves inflammation that can lead to pain and stiffness.
- Spondylolysis: This condition involves a stress fracture in one of the vertebrae, often due to repetitive stress or trauma. It differs from spondylosis, which involves degenerative changes.
- Spondylolisthesis: This occurs when one vertebra slips over another, which can result from spondylolysis or degenerative changes like those seen in spondylosis.
frequently asked questions
What is the main cause of spondylosis?
The primary cause of spondylosis is aging, as the spine undergoes natural degenerative changes over time. Mechanical stress and lifestyle factors, such as poor posture and lack of physical activity, can also contribute to its progression.
Can spondylosis be cured?
While spondylosis cannot be cured, its symptoms can be effectively managed through lifestyle changes, physical therapy, and medication. These interventions aim to alleviate pain, improve mobility, and enhance quality of life.
How does spondylosis differ from other spinal conditions?
Spondylosis is characterized by degenerative changes in the spine, whereas conditions like spondylitis involve inflammation. Spondylolysis involves a stress fracture, and spondylolisthesis involves vertebral slippage. Understanding these differences is crucial for proper diagnosis and treatment.
What are the treatment options for spondylosis?
Treatment for spondylosis typically includes pain management through medications, physical therapy to strengthen supporting muscles, and ergonomic adjustments. In severe cases, surgical intervention may be necessary to relieve nerve compression or stabilize the spine.
Is spondylosis preventable?
While the aging process cannot be prevented, maintaining a healthy lifestyle with good posture, regular exercise, and proper ergonomics can help reduce the risk of developing spondylosis or slow its progression.
By understanding these aspects of spondylosis, individuals can better manage their condition and work towards maintaining a healthy spine throughout their lives.