When it comes to spinal health, much of the focus tends to be on the more commonly affected areas such as the lumbar (lower back) or cervical (neck) regions. However, a herniated disc in the middle of the back, known as the thoracic region, can also be a source of significant discomfort and disability. Despite being less prevalent, this condition can cause severe pain and disrupt daily activities, making it essential to shed light on its symptoms and treatment options.
The importance of understanding thoracic disc herniation
Understanding the nuances of a thoracic herniated disc is crucial for anyone experiencing unexplained mid-back pain. This condition can be particularly insidious, as its symptoms may not always be immediately apparent or may mimic other issues. Ignoring these signs can lead to severe complications, including chronic pain or even neurological deficits if the spinal cord becomes compressed. Therefore, gaining a clear understanding of the symptoms and potential treatments is vital for effective management and prevention of further harm.
The impact of a herniated disc in the middle of the back extends beyond physical discomfort. It can significantly alter one's quality of life, affecting everything from work performance to personal relationships. Simple tasks like lifting objects, sitting for extended periods, or even breathing deeply can become challenging. Therefore, early recognition and intervention are key to preserving mobility and maintaining a good quality of life.
What you will learn
This blog post will delve into the intricate details of thoracic herniated discs, providing you with a comprehensive understanding of this condition. You will learn about the common symptoms that accompany a herniated disc in the middle of the back, such as upper back pain, radiating discomfort along the ribs, and potential numbness or tingling. We will also explore the anatomy of the thoracic spine to help you understand how herniation occurs in this specific region.
Furthermore, we will discuss the primary causes and risk factors associated with thoracic disc herniation, including degenerative disc disease, trauma, and lifestyle factors. Finally, we will outline the various treatment options available, ranging from non-surgical methods like physical therapy and pain management to surgical interventions for more severe cases.
By the end of this post, you will have a thorough understanding of the complexities of a herniated disc in the middle of the back, empowering you to make informed decisions about your health and well-being.
Symptoms and diagnosis of a thoracic herniated disc
The symptoms of a herniated disc in the middle of the back can vary widely, often depending on the severity and specific location of the herniation. Commonly, individuals may experience persistent upper back pain that can be exacerbated by certain movements or prolonged activities. This pain often radiates along the ribs or chest wall, sometimes mimicking other conditions such as cardiac issues or respiratory problems, which can complicate diagnosis.
Numbness and tingling are also frequent symptoms, typically manifesting in the torso or upper limbs. In more severe cases, a thoracic herniated disc can lead to myelopathy, a condition where the spinal cord is compressed, potentially resulting in weakness or paralysis. This underscores the importance of early diagnosis and intervention.
Diagnosing a thoracic herniated disc typically involves imaging studies, with MRI and CT scans being the primary tools. These imaging techniques provide detailed views of the spine, allowing for precise identification of herniated discs and any associated spinal cord compression. A thorough clinical evaluation by a healthcare professional is also crucial to rule out other potential causes of symptoms and to develop an effective treatment plan.
Understanding the anatomy of the thoracic spine
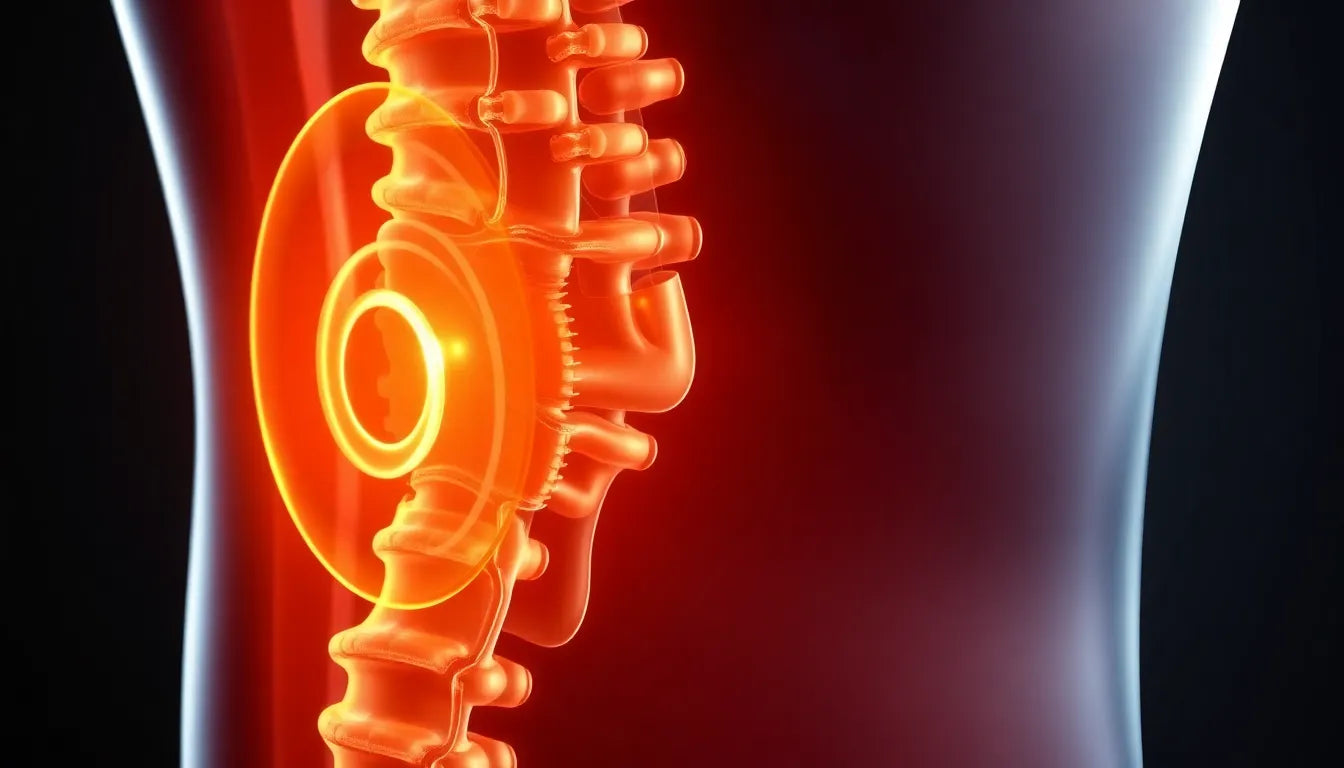
The thoracic spine comprises 12 vertebrae, labeled T1 through T12, and is located between the cervical and lumbar regions of the spine. This section of the spine is unique in its structure and function, as it is designed to provide stability and support to the upper body while protecting the spinal cord. The rib cage attaches to the thoracic vertebrae, which limits the range of motion in this region compared to the more flexible cervical and lumbar areas.
Herniation in the thoracic spine occurs when the inner gel-like core of a disc pushes through its outer layer, potentially pressing on nearby nerves or the spinal cord itself. This can happen due to various factors, including degenerative changes, trauma, or repetitive stress. Understanding the anatomy of the thoracic spine is essential for comprehending how and why herniations occur in this region, as well as for planning appropriate treatment strategies.
Causes and risk factors for thoracic disc herniation
Several factors can contribute to the development of a herniated disc in the middle of the back. Degenerative disc disease is a common cause, where the discs naturally lose hydration and elasticity with age, making them more susceptible to herniation. Trauma or injury, such as from a fall or accident, can also lead to disc herniation by causing sudden pressure on the spine.
Poor posture, especially when combined with repetitive strain from activities like heavy lifting or prolonged sitting, can exacerbate the risk of developing a herniated disc. Additionally, certain lifestyle factors, including a sedentary lifestyle and obesity, can increase the strain on the spinal discs, making them more prone to damage.
Genetic predisposition may also play a role, with some individuals being more susceptible to disc degeneration and herniation due to inherited traits. Understanding these risk factors is crucial for both preventing and managing thoracic disc herniation, as lifestyle modifications and early interventions can significantly reduce the likelihood of developing this condition.
Treatment options for herniated discs in the middle of the back
When managing a herniated disc in the middle of the back, a range of treatment options is available, tailored to the severity of the condition and the specific needs of the patient. Non-surgical treatments are often the first line of defense, aiming to alleviate pain and improve function without invasive procedures.
Non-surgical treatments
Rest and physical therapy are fundamental components of conservative treatment. Rest allows the affected area to heal, while physical therapy focuses on strengthening the back muscles and improving flexibility, which can reduce the risk of further injury. Pain management is another critical aspect, with non-steroidal anti-inflammatory drugs (NSAIDs) and, in some cases, narcotics prescribed to manage discomfort. Anti-inflammatory agents and epidural steroid injections can provide relief by reducing inflammation around the herniated disc and alleviating pressure on the nerves.
While these treatments can be effective, they come with limitations. Rest and medication alone may not address the underlying cause of the herniation, and long-term use of narcotics can lead to dependency. Therefore, a comprehensive approach involving multiple therapies is often recommended.
Surgical options
When non-surgical treatments fail to provide relief or if there is significant spinal cord compression, surgical intervention may be necessary. Common procedures include laminotomy and discectomy, which involve removing part of the vertebra or disc to relieve pressure on the spinal cord or nerves. Minimally invasive techniques, such as Video Assisted Thoracic Surgery (VATS), are increasingly popular due to their reduced recovery times and lower risk of complications compared to traditional open surgery.
Each surgical method has its own outcomes and recovery timelines, which should be discussed in detail with a healthcare provider to determine the best option for the patient's specific condition.
Lifestyle changes and prevention strategies
Preventing a herniated disc in the middle of the back involves adopting lifestyle changes that reduce strain on the spine. Here are some practical tips:
- Maintain good posture, especially when sitting for long periods.
- Engage in regular exercise to strengthen back and core muscles.
- Incorporate ergonomic adjustments at work and home to minimize stress on the spine.
- Avoid heavy lifting, or use proper techniques if lifting is necessary.
- Maintain a healthy weight to reduce pressure on the spinal discs.
By integrating these strategies into daily life, individuals can significantly decrease their risk of developing thoracic disc herniation and enhance their overall spinal health.
Frequently asked questions
What is a thoracic herniated disc?
A thoracic herniated disc occurs when the inner core of a spinal disc in the middle of the back protrudes through its outer layer, potentially pressing on nearby nerves or the spinal cord.
What are the common symptoms?
Key symptoms include upper back pain, radiating pain along the ribs or chest wall, numbness, tingling, and in severe cases, myelopathy or paralysis.
How is it diagnosed?
Diagnosis typically involves MRI and CT scans, which provide detailed images of the spine, along with a thorough clinical evaluation to assess symptoms and rule out other conditions.
What are the treatment options?
Treatment options range from non-surgical methods like rest, physical therapy, and pain management with medications to surgical interventions such as laminotomy, discectomy, and minimally invasive techniques like VATS.
Can lifestyle changes help prevent herniation?
Yes, maintaining good posture, regular exercise, ergonomic adjustments, and a healthy weight can help prevent thoracic herniation.
When should I see a doctor?
It is advisable to seek medical attention if you experience persistent or severe symptoms, such as significant pain, numbness, or weakness, as early intervention can prevent further complications.