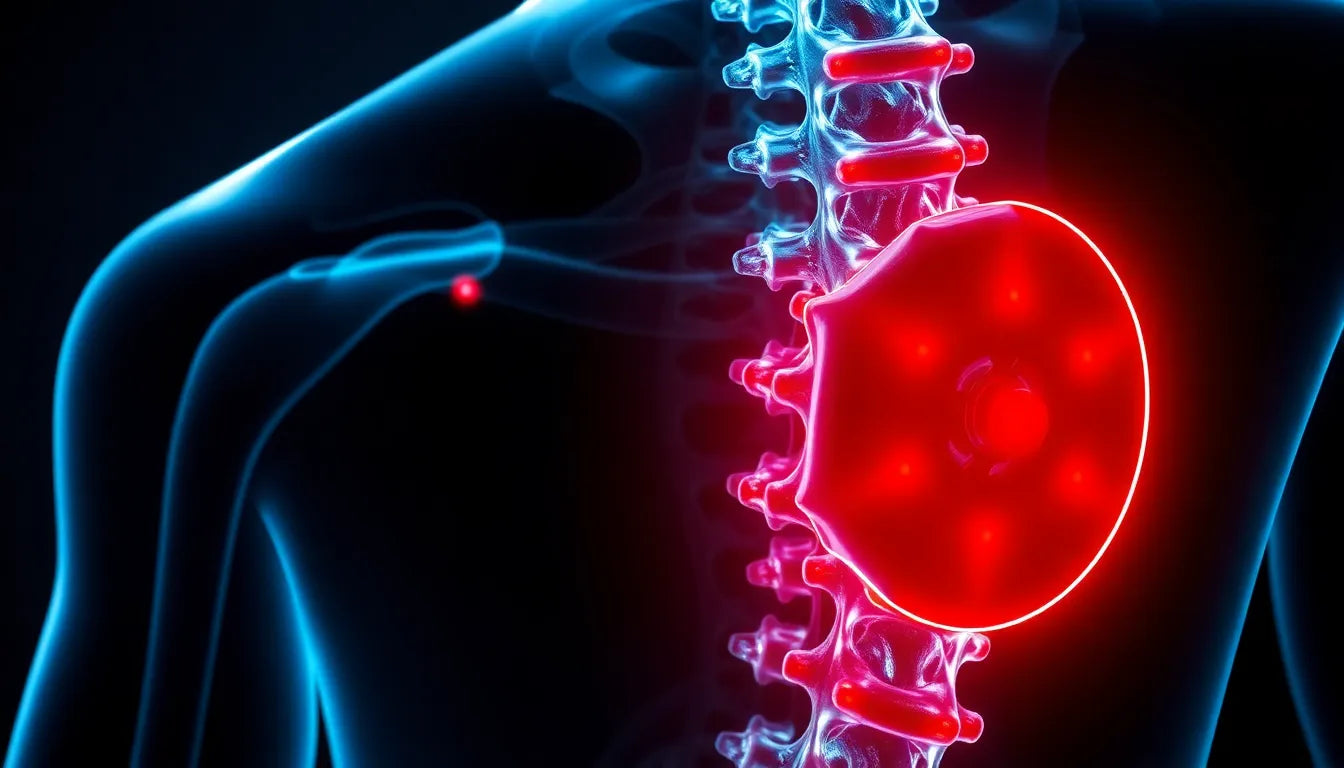
A herniated disc and sacroiliac (SI) joint pain are two common conditions that can significantly impact an individual's quality of life. A herniated disc occurs when the soft inner gel of a spinal disc pushes through a crack in the tougher exterior casing, potentially pressing on nearby nerves and causing pain. On the other hand, the sacroiliac joint connects the spine to the pelvis, and pain in this area can result from inflammation or dysfunction of the joint. Both conditions can lead to discomfort, reduced mobility, and difficulty performing everyday activities.
Understanding the connection between herniated discs and SI joint pain
Understanding the link between herniated discs and SI joint pain is crucial for effective diagnosis and treatment. These conditions often share overlapping symptoms, such as lower back pain and discomfort radiating into the legs, which can complicate the diagnostic process. By recognizing the relationship between these two conditions, healthcare providers can more accurately identify the underlying issues and develop targeted treatment plans that address the root cause of the pain.
Due to the complexity of these conditions, misdiagnosis is not uncommon. Symptoms of a herniated disc can mimic those of SI joint pain and vice versa, leading to potential delays in receiving appropriate treatment. This makes it even more important for individuals experiencing persistent back pain to seek a thorough evaluation from a medical professional who can distinguish between the two and recommend the most effective course of action.
Purpose of this post
This post aims to shed light on the intricate relationship between herniated discs and SI joint pain. Readers will gain insights into the symptoms associated with each condition, the diagnostic methods used to differentiate them, and the various treatment options available. By the end of this post, you will have a clearer understanding of these conditions and be better equipped to seek the right medical advice and interventions.
Stay tuned as we delve deeper into the symptoms, diagnosis, and treatment strategies that can help manage these conditions effectively. Whether you're dealing with back pain yourself or supporting someone who is, this post will provide valuable information to guide you in navigating the complexities of herniated discs and SI joint pain.
Symptoms of herniated discs and si joint pain
When distinguishing between herniated discs and SI joint pain, it is important to understand the specific symptoms associated with each condition. Herniated discs often present with localized back pain, which can extend to leg pain, numbness, and tingling sensations. This occurs because the herniated material can press on nearby nerves, disrupting normal nerve function. The intervertebral discs, which act as cushions between the vertebrae, play a critical role in maintaining spinal flexibility and absorbing shock. When these discs herniate, they can significantly impair movement and cause discomfort.
In contrast, SI joint pain typically manifests as lower back pain that can radiate to the buttocks and down the legs. The sacroiliac joint, which connects the spine to the pelvis, is crucial for transferring weight and stabilizing the body during movement. Dysfunction or inflammation in this joint can lead to pain and reduced mobility, often exacerbated by activities such as standing, walking, or climbing stairs. Understanding these distinct symptoms is vital for accurate diagnosis and effective treatment.
Diagnosing herniated discs and si joint pain
Accurate diagnosis of herniated discs and SI joint pain requires a combination of clinical examinations and imaging techniques. During a clinical examination, healthcare providers may perform specific physical tests to differentiate between the two conditions. For example, the straight leg raise test can help identify nerve root irritation caused by a herniated disc, while the FABER test (Flexion, Abduction, and External Rotation) is often used to assess SI joint dysfunction.
Imaging techniques such as MRI and CT scans play a crucial role in diagnosing these conditions. An MRI can provide detailed images of the spine, revealing disc herniation, while a CT scan can highlight inflammation or abnormalities in the SI joint. These imaging methods help healthcare providers pinpoint the exact cause of pain, allowing for more targeted treatment plans.
Exploring the correlation between herniated discs and si joint pain
Research has shown a notable correlation between herniated discs and SI joint dysfunction. Studies published in medical journals like PubMed indicate that SI joint dysfunction is relatively common in patients with herniated discs, often due to altered biomechanics and compensatory movements. When a herniated disc affects the spine's stability, it can lead to increased stress on the SI joint, potentially resulting in pain and dysfunction.
This interconnectedness underscores the importance of a comprehensive approach to diagnosis and treatment. By considering the potential link between these conditions, healthcare providers can develop more effective strategies to address the root causes of pain and improve patient outcomes. Understanding the biomechanics involved can also guide physical therapy and rehabilitation efforts, helping patients regain function and reduce pain.
In conclusion, recognizing the distinct symptoms and diagnostic methods for herniated discs and SI joint pain is crucial for effective management. By exploring the correlation between these conditions, healthcare providers can offer more targeted treatments that address the underlying issues, ultimately improving patients' quality of life. Stay tuned for the next part of this series, where we will delve into the various treatment options and strategies for managing and preventing pain associated with these conditions.
Treatment options for herniated discs and SI joint pain
When it comes to managing herniated discs and SI joint pain, a comprehensive approach that includes both non-operative and operative treatments can be crucial for effective relief and recovery. Non-operative treatments are often the first line of defense and can significantly improve symptoms for many patients.
Non-operative treatments typically involve a combination of physical therapy, chiropractic care, and pain management strategies. Physical therapy focuses on strengthening the muscles around the spine and pelvis, improving flexibility, and teaching proper body mechanics to reduce strain on the affected areas. Chiropractic care may help realign the spine and pelvis to alleviate pressure on nerves and joints. Pain management can include medications such as NSAIDs or corticosteroid injections to reduce inflammation and pain. Additionally, ergonomic aids like supportive cushions or braces can assist in maintaining proper posture and reducing stress on the spine and SI joint during daily activities.
For patients who do not respond to conservative treatments, operative treatments may be considered. Surgical options include procedures like discectomy, where the herniated portion of the disc is removed to relieve nerve pressure, or SI joint fusion, which stabilizes the joint by fusing the bones together. Post-surgical rehabilitation is essential to ensure a successful recovery, focusing on gradually restoring strength and mobility while preventing future injuries.
Managing and preventing pain
Preventing and managing pain associated with herniated discs and SI joint issues often requires lifestyle changes and proactive measures. Regular exercise, including low-impact activities like swimming or walking, can help maintain a healthy weight and improve overall spinal health. Incorporating specific exercises that target core stability and flexibility can also be beneficial.
Ergonomic adjustments at home and work, such as using an ergonomic chair or adjusting the height of your workstation, can help maintain proper posture and reduce strain on the back and pelvis. Early intervention and regular medical check-ups are vital in managing symptoms before they become severe. By addressing pain early and adhering to a tailored treatment plan, individuals can significantly improve their quality of life and reduce the risk of chronic pain.
Frequently Asked Questions
Can a herniated disc cause sacroiliac pain?
Yes, a herniated disc can contribute to sacroiliac pain. When a herniated disc affects the biomechanics of the spine, it can lead to compensatory movements that place additional stress on the SI joint, potentially causing pain and dysfunction.
How is sacroiliac joint pain diagnosed?
Diagnosing SI joint pain typically involves a combination of physical examinations and imaging techniques. Tests like the FABER test can help assess SI joint dysfunction, while imaging methods such as MRI or CT scans can provide detailed views of joint inflammation or abnormalities.
What are the risk factors for developing these conditions?
Risk factors for herniated discs and SI joint pain include age, occupation, and lifestyle. Activities that involve heavy lifting, prolonged sitting, or repetitive movements can increase the risk. Additionally, factors like obesity, previous injuries, and poor posture can contribute to these conditions.
Are there long-term effects of untreated herniated discs or SI joint pain?
Untreated herniated discs or SI joint pain can lead to chronic pain, reduced mobility, and potentially permanent nerve damage. Timely diagnosis and treatment are crucial to prevent these long-term complications and improve patient outcomes.
What role does posture play in these conditions?
Poor posture can exacerbate symptoms of herniated discs and SI joint pain by increasing stress on the spine and pelvis. Maintaining good posture through ergonomic support and regular exercise is essential in managing and preventing these conditions.