A herniated disc, often referred to as a slipped or ruptured disc, is a common spinal condition that affects many adults worldwide. This condition arises when one of the intervertebral discs, which act as cushions between the vertebrae, becomes damaged and its inner gel-like core protrudes through the outer layer. Recognizing the symptoms of a herniated disc early is crucial, as timely intervention can prevent the condition from worsening and reduce the risk of long-term complications.
understanding the spine and disc anatomy
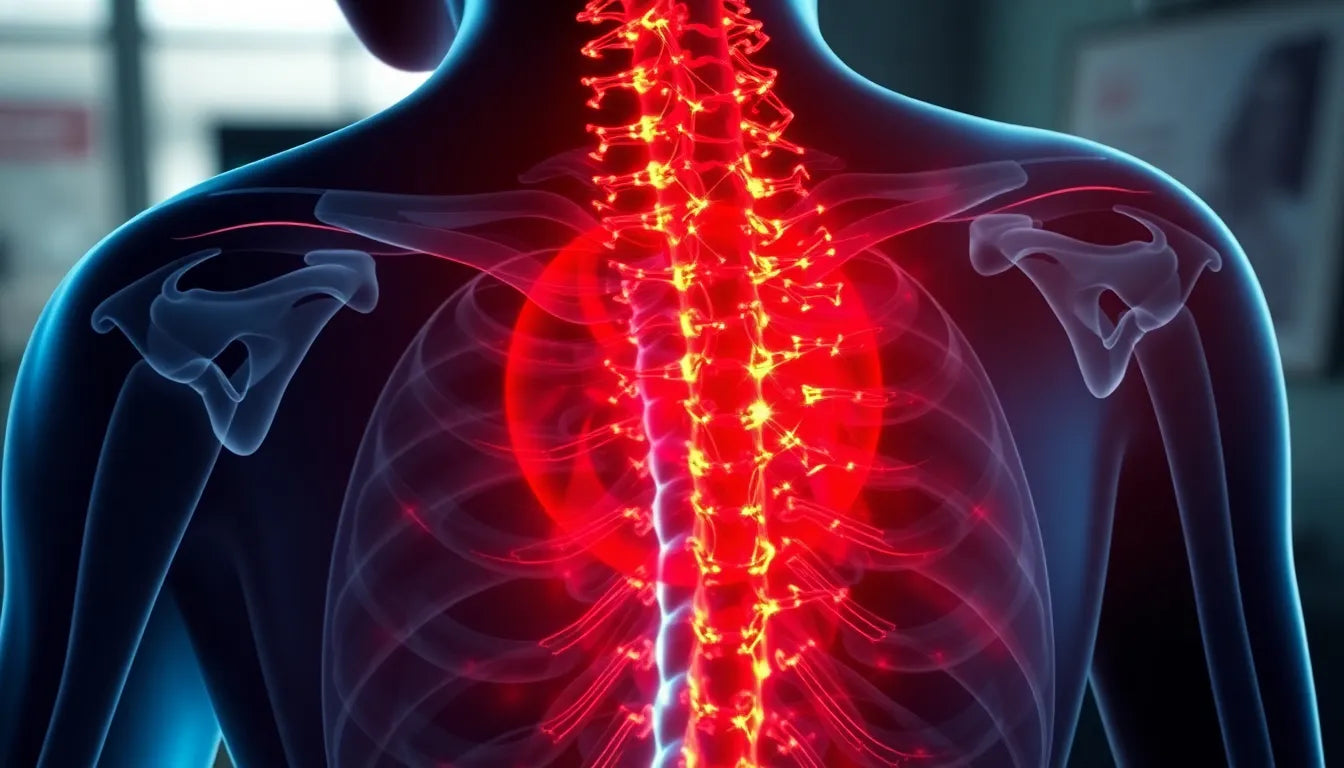
The human spine is a complex structure composed of vertebrae, intervertebral discs, nerves, and supporting muscles and ligaments. The intervertebral discs serve as shock absorbers, allowing for flexibility and movement while protecting the spinal cord. These discs have a tough outer layer called the annulus fibrosus and a soft, gel-like center known as the nucleus pulposus. A herniated disc occurs when the nucleus pulposus pushes through a tear or weak spot in the annulus fibrosus. It’s important to distinguish this from a bulging disc, where the disc protrudes but the nucleus remains contained within the annulus.
the silent nature of symptoms
Symptoms of a herniated disc can be surprisingly subtle and are often overlooked or misattributed to other conditions. This is why the condition is sometimes referred to as having "silent" symptoms. Many individuals may experience mild discomfort or no symptoms at all, while others may suffer from severe pain or neurological issues. The variability in symptoms is largely due to the location of the herniation and the extent of nerve involvement. Early detection and awareness are essential, as ignoring the signs can lead to more severe issues, such as chronic pain or permanent nerve damage. Being informed about the silent signs of a herniated disc can empower individuals to seek medical advice promptly, ensuring better outcomes and quality of life.
common symptoms of a herniated disc
One of the most prevalent symptoms of a herniated disc is back pain. This pain can range from a dull ache to a sharp, intense sensation, often exacerbated by movement or prolonged sitting. It's crucial to differentiate between localized pain, which is confined to the area of the herniation, and radiating pain, commonly known as sciatica. Sciatica occurs when the herniated disc compresses a nerve root, causing pain to travel down the leg, sometimes reaching the foot. This type of radiating pain is a telltale sign of nerve involvement and should not be ignored.
neurological symptoms and nerve compression
Beyond pain, herniated discs can lead to neurological symptoms such as numbness, tingling, and muscle weakness in the limbs. These symptoms arise when the herniated material presses on nearby nerves, disrupting normal nerve function. For instance, a herniation in the lumbar region might cause symptoms in the legs, while a cervical herniation could affect the arms and shoulders. It's essential to understand that these neurological symptoms indicate nerve compression, which, if left untreated, can lead to more severe complications such as permanent nerve damage.
stages of herniation
The progression of a herniated disc can be divided into several stages, starting with disc degeneration. Initially, the disc may lose its water content and elasticity, leading to small tears in the outer layer. This is followed by the prolapse stage, where the inner core begins to push against the weakened annulus fibrosus. As the condition advances, the extrusion stage occurs, with the nucleus pulposus breaking through the outer layer. Finally, in the sequestration stage, fragments of the nucleus may separate from the disc entirely. Understanding these stages helps in identifying the severity of the condition and planning appropriate treatment strategies.
differences between lumbar and cervical herniation
While herniated discs can occur anywhere along the spine, lumbar and cervical herniations are the most common. Lumbar herniations typically lead to lower back pain and sciatica, affecting the lower body. In contrast, cervical herniations can cause neck pain, headaches, and pain radiating to the shoulders and arms. It's important to note that cervical herniations may also lead to more severe symptoms such as difficulty with fine motor skills or balance issues due to their proximity to the brain and spinal cord. Recognizing these differences is crucial for accurate diagnosis and treatment.
when to seek medical help
While many cases of herniated discs can be managed with conservative treatments, certain symptoms warrant immediate medical attention. Red flags include severe or worsening pain, loss of bladder or bowel control, and profound weakness in the limbs. These symptoms may indicate a condition called cauda equina syndrome, a rare but serious disorder that requires urgent surgical intervention. If you experience any of these symptoms, it's imperative to seek medical help promptly to prevent permanent damage.
potential causes and risk factors of a herniated disc
A herniated disc can result from various factors, with age-related wear and tear being the most common cause. As we age, the intervertebral discs lose water content, making them less flexible and more prone to tearing or rupturing with even minor strains or twists. Injuries, such as a fall or a blow to the back, can also lead to disc herniation. Additionally, certain lifestyle factors increase the risk of developing a herniated disc, including obesity, which adds stress to the spine, and a sedentary lifestyle, which weakens the muscles supporting the spine. Genetics may also play a role, as some individuals inherit a predisposition to developing herniated discs.
treatment options for herniated discs
For many individuals, herniated disc symptoms can be managed with non-surgical treatments. Physical therapy is often recommended to strengthen the muscles around the spine, improve flexibility, and reduce pain. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help relieve pain and reduce inflammation. Lifestyle changes, including maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate symptoms, are crucial for managing the condition. In severe cases where conservative treatments fail to provide relief, surgical options, such as a discectomy or spinal fusion, may be considered. Consulting with a healthcare professional is essential to determine the most appropriate treatment plan based on individual symptoms and overall health.
conclusion
Recognizing the symptoms of a herniated disc early is vital for preventing further complications and ensuring effective treatment. By understanding the potential causes, risk factors, and available treatment options, individuals can take proactive steps to manage their condition and improve their quality of life. Paying attention to your body and seeking medical advice if you suspect a herniated disc can lead to better outcomes and prevent long-term damage. Remember, early intervention is key to maintaining spinal health and overall well-being.
Frequently Asked Questions
What are the stages of a herniated disc?
The stages of a herniated disc begin with disc degeneration, where the disc loses its water content and elasticity. This is followed by the prolapse stage, where the inner core starts pushing against the outer layer. In the extrusion stage, the nucleus pulposus breaks through the annulus fibrosus. Finally, in the sequestration stage, fragments of the nucleus may separate from the disc entirely.
How do you know if you have a herniated disc?
Common symptoms of a herniated disc include back pain, radiating pain down the legs or arms, numbness, tingling, and muscle weakness. If you experience these symptoms, it is advisable to seek a medical evaluation for a definitive diagnosis.
Can a herniated disc heal on its own?
In some cases, a herniated disc can heal on its own with time and conservative treatment. Factors influencing recovery include the severity of the herniation, the individual's overall health, and adherence to recommended lifestyle changes and treatment plans.
What activities should be avoided with a herniated disc?
Activities that should be avoided with a herniated disc include heavy lifting, twisting motions, high-impact exercises, and prolonged sitting or standing. Safe alternatives include low-impact activities like walking, swimming, and using an elliptical machine.
Is surgery always necessary for a herniated disc?
Surgery is not always necessary for a herniated disc. Most cases can be managed with non-surgical treatments. Surgery is typically considered when conservative treatments fail to relieve symptoms or if there are severe symptoms such as significant weakness or loss of bladder control.