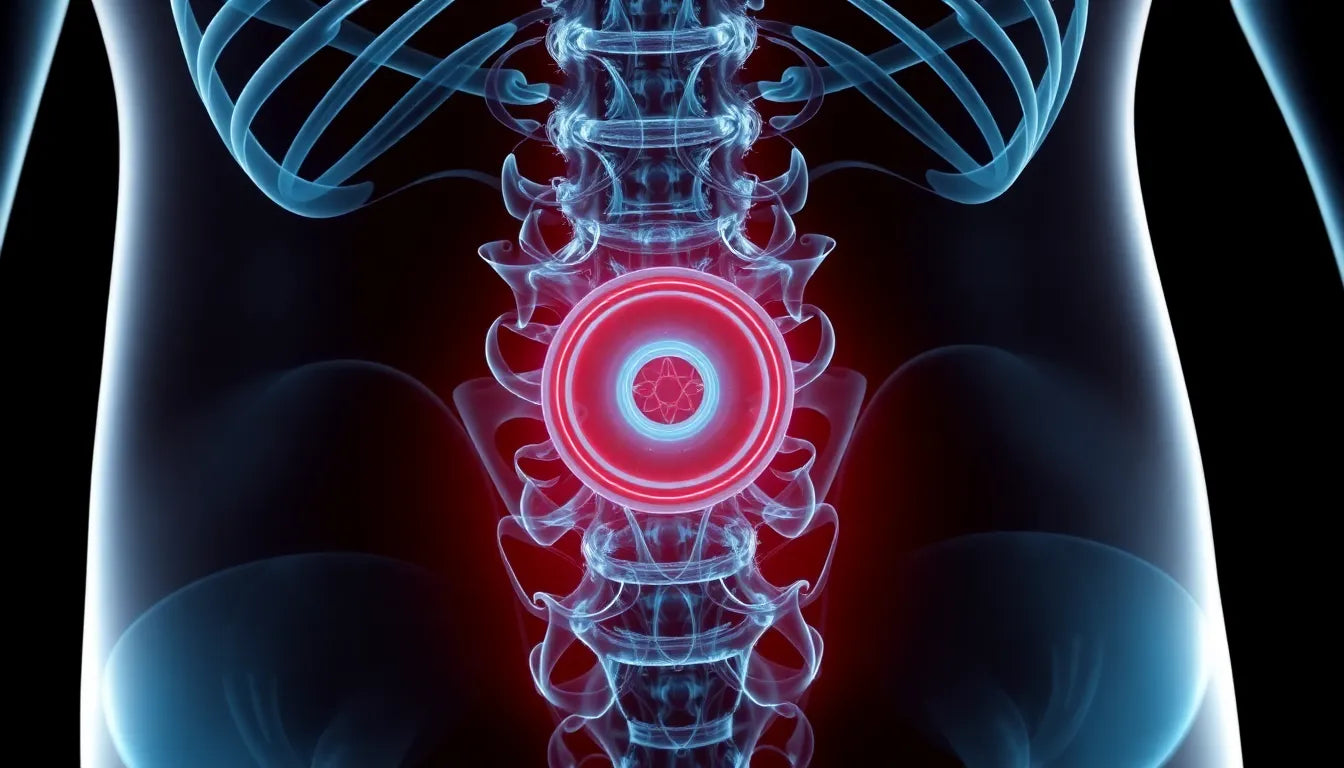
A back herniated disc, often referred to as a slipped or ruptured disc, is a condition that occurs when the nucleus pulposus, the gel-like center of a spinal disc, protrudes through a tear in the annulus fibrosus, the disc's tough outer layer. This protrusion can press against spinal nerves, leading to discomfort and a range of symptoms. While herniated discs can occur in any part of the spine, they are most prevalent in the lumbar region, which is the lower back. This area bears much of the body's weight and is involved in many of our daily movements, making it particularly susceptible to disc herniation.
Understanding the prevalence and impact
Herniated discs are surprisingly common, with studies suggesting that a significant portion of the population will experience this condition at some point in their lives. The lumbar region is especially vulnerable due to its role in supporting the upper body and facilitating movements such as bending and twisting. The symptoms of a herniated disc can vary depending on the location and severity of the herniation, but they often include localized pain, numbness, tingling, and muscle weakness. These symptoms can significantly impact daily life, affecting everything from basic mobility to the ability to perform routine tasks.
The importance of addressing back pain
Addressing back pain promptly is crucial for maintaining quality of life and preventing further complications. Early diagnosis and management of a herniated disc can alleviate symptoms and reduce the risk of long-term damage. This blog aims to provide a comprehensive guide on managing a herniated disc effectively, offering insights into both conservative and surgical treatment options. By understanding the condition and exploring various management strategies, individuals can make informed decisions about their health and well-being.
Causes and risk factors of a herniated disc
Understanding the causes and risk factors associated with a back herniated disc is crucial for both prevention and management. Activities that significantly increase spinal disc pressure, such as bending and lifting with a rounded back, are common culprits. These movements can lead to small tears in the annulus fibrosus, allowing the nucleus pulposus to protrude. Additionally, prolonged sitting, especially without proper lumbar support, can exacerbate the pressure on spinal discs, further increasing the risk of herniation.
Age-related degeneration is another significant factor. As we age, the spinal discs naturally lose some of their water content, making them less flexible and more prone to tearing under pressure. Repetitive strain from certain occupations or sports can also contribute to the wear and tear of spinal discs, leading to a higher likelihood of herniation. Recognizing these risk factors can help in adopting preventive measures to protect your spine.
Identifying symptoms and the diagnosis process
Identifying the symptoms of a herniated disc early can significantly impact the treatment outcome. Common symptoms include localized back pain, sciatica (pain radiating down the leg), numbness, and muscle weakness. These symptoms occur due to the pressure exerted by the herniated disc on nearby spinal nerves, which can vary in intensity based on the severity and location of the herniation.
Diagnosis typically begins with a clinical evaluation, where a healthcare provider will review your medical history and perform a physical examination. Key diagnostic tests include the straight-leg raising test, which helps identify nerve root compression indicative of a lumbar herniation. Imaging tests such as MRI and CT scans are often employed to confirm the diagnosis and assess the extent of the herniation. In some cases, a provocation discography may be used to pinpoint the exact source of pain, although this is less common.
Exploring conservative treatment options
For many individuals, conservative treatment options can effectively manage a herniated disc. Physical therapy plays a pivotal role, focusing on exercises that strengthen the back muscles and improve flexibility. A physical therapist can design a tailored program to address your specific needs, helping to alleviate pressure on the affected disc and reduce pain.
Medications are often used in conjunction with physical therapy to manage pain and inflammation. Over-the-counter pain relievers and anti-inflammatory drugs can provide relief, but it's essential to use them as directed by a healthcare professional to avoid potential side effects.
Rest and lifestyle modifications are also critical components of conservative treatment. Ensuring proper ergonomics in daily activities, such as maintaining good posture and using supportive seating, can prevent further strain on the spine. Additionally, avoiding activities that exacerbate symptoms, such as heavy lifting and twisting motions, is crucial for recovery.
By understanding the causes, symptoms, and conservative treatment options for a back herniated disc, individuals can take proactive steps towards effective management and recovery. In the next section, we will delve into surgical interventions and long-term management strategies, providing a comprehensive guide to navigating this common spinal condition.
Surgical interventions for herniated discs
While many individuals find relief through conservative treatments, there are cases where surgical intervention becomes necessary to manage a back herniated disc. Surgery is typically considered when symptoms are severe, disabling, or when conservative treatments have failed to provide adequate relief over a significant period.
One of the surgical options available is total disc replacement. This procedure involves removing the damaged disc and replacing it with an artificial one, aiming to maintain normal disc height and motion. Total disc replacement can be effective for some patients, offering pain relief and improved mobility. However, it is crucial to consult with a spine specialist to determine if this option is suitable, as not all patients are candidates for this surgery.
Long-term management and recovery strategies
Recovery from a herniated disc, whether through conservative or surgical means, involves ongoing management to prevent recurrence and maintain spine health. For many, recovery is possible without surgery, especially with a comprehensive approach that includes physical therapy, lifestyle modifications, and ergonomic adjustments.
Long-term strategies focus on strengthening the core and back muscles, maintaining a healthy weight, and practicing good posture. Regular physical activity tailored to your condition can help keep the spine flexible and reduce the risk of future disc herniation. Additionally, adopting ergonomic solutions in the workplace and at home, such as using supportive chairs and adjusting desk heights, can significantly impact spine health.
Ergonomics and prevention
Ergonomics plays a vital role in both managing and preventing herniated discs. Implementing ergonomic aids can help reduce strain on the spine during daily activities. For example, ergonomic chairs that provide lumbar support can alleviate pressure on the lower back, while posture supports can encourage proper alignment.
Incorporating these solutions into your daily routine can help prevent the onset of herniated discs and support recovery if you are already experiencing symptoms. It's essential to evaluate your environment and make necessary adjustments to ensure that your spine is adequately supported throughout the day.
Frequently asked questions
Can a herniated disc heal without surgery?
Yes, many cases of a herniated disc improve with conservative treatment methods such as physical therapy, medications, and lifestyle modifications. Surgery is usually considered only when these options fail to provide relief.
What activities should be avoided with a herniated disc?
Activities that involve heavy lifting, twisting motions, and prolonged sitting without proper support should be avoided, as they can exacerbate symptoms and hinder recovery.
How long does it take to recover from a herniated disc?
Recovery time varies depending on the severity of the herniation and the treatment approach. Some individuals may experience improvement within a few weeks, while others may take several months to recover fully.
When should I see a doctor for a herniated disc?
If you experience severe pain, numbness, or muscle weakness that affects your daily activities, it is important to seek medical attention to receive a proper diagnosis and treatment plan.
Are there any exercises that can help with a herniated disc?
Yes, specific exercises designed to strengthen the back and improve flexibility can be beneficial. However, it is crucial to perform these exercises under the guidance of a healthcare professional to ensure they are safe and effective for your condition.
Sources
- "Disc Herniation." NCBI/StatPearls.
- "Lumbar disc herniation: Epidemiology, clinical and radiologic ..." ScienceDirect.
- "Herniated disk - Diagnosis and treatment." Mayo Clinic.
- "Management of Lumbar Disc Herniation: A Systematic Review." PMC.
- "Clinical Evaluation and Treatment Options for Herniated Lumbar Disc." AAFP.
- "Herniated Disc Treatment Options." Cuellar Spine.
- "Disc herniation." Wikipedia.