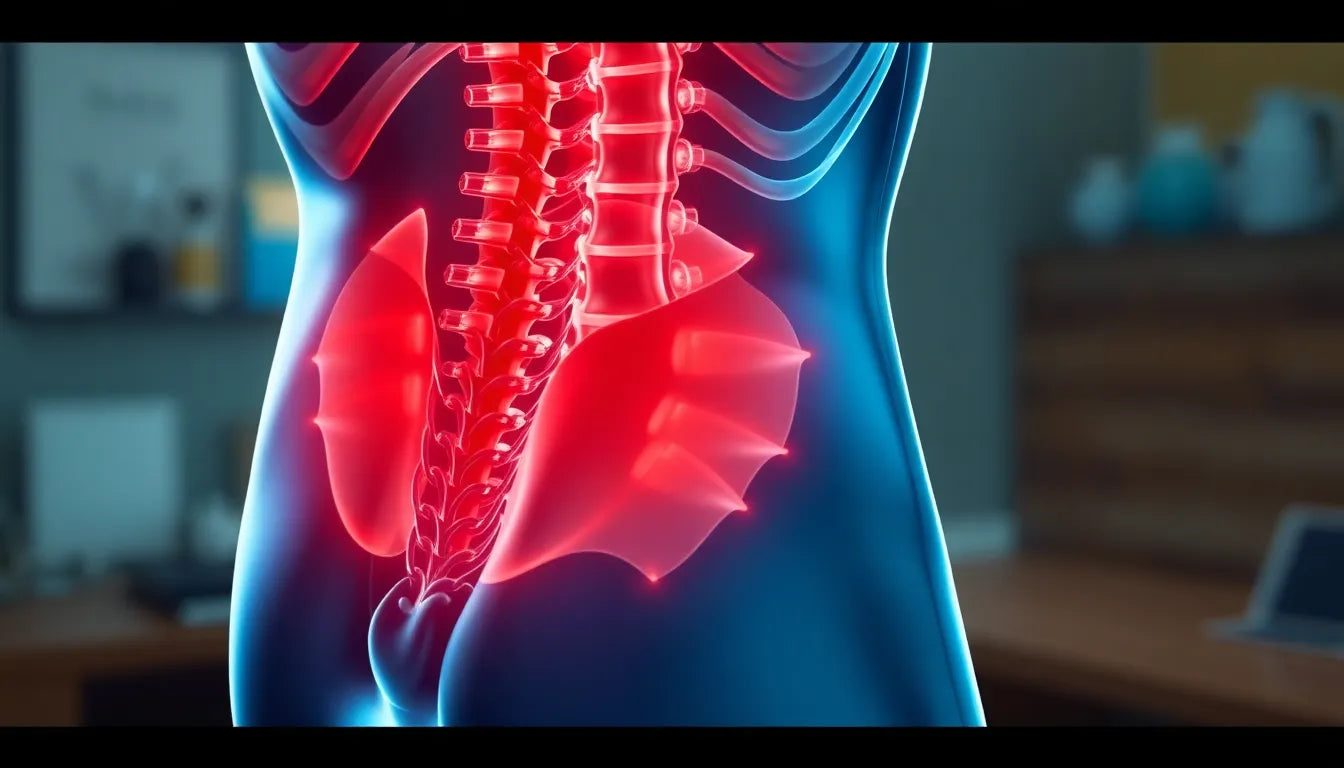
When it comes to understanding what a herniated disc feels like, the journey is often shrouded in mystery and complexity. For those who haven't experienced it, the term might conjure up images of debilitating pain and immobility. However, the reality is much more nuanced. A herniated disc occurs when the cushioning material between the vertebrae in the spine displaces, potentially pressing on nearby nerves. This can lead to a variety of symptoms that are crucial to recognize for timely diagnosis and treatment.
Understanding the herniated disc
The spine is made up of a series of bones called vertebrae, cushioned by discs that act as shock absorbers. When a disc becomes herniated, its inner gel-like core pushes through the tougher exterior, often leading to nerve irritation. The sensation can range from mild discomfort to severe, incapacitating pain, depending on the location and severity of the herniation. Recognizing these symptoms early is key to managing the condition effectively and preventing further complications.
Common misconceptions about herniated discs
One of the most prevalent misconceptions about herniated discs is the belief that they always cause severe pain. While it's true that some individuals experience intense discomfort, others may only feel mild symptoms or none at all. This variability can make it challenging to identify a herniated disc based solely on pain levels. Additionally, some people assume that the condition is easily identifiable through pain alone, but the symptoms can be subtle and mimic other conditions, leading to misdiagnosis or delayed treatment.
It's important to note that not everyone with a herniated disc will experience noticeable discomfort. In some cases, the condition is discovered incidentally through imaging tests conducted for unrelated issues. This phenomenon underscores the importance of understanding the full spectrum of symptoms associated with herniated discs, as they can vary widely from person to person.
In summary, recognizing the signs of a herniated disc is crucial for seeking appropriate medical care. While the condition can present with a range of symptoms, understanding its nature and common misconceptions can help individuals better navigate their health journey. As we delve deeper into the specifics of herniated disc sensations, we'll explore the different types of pain and how they manifest based on the location of the disc within the spine.
General sensation and pain quality of a herniated disc
Experiencing a herniated disc can be likened to enduring a sharp, burning, or stinging pain that often radiates from the affected area of the spine into the limbs. This pain is a result of the displaced disc material pressing on nearby nerves. The sensation can be quite intense, often described as a shooting pain that travels along the nerve path. Accompanying symptoms might include numbness, tingling, or muscle weakness, which can further complicate daily activities and reduce quality of life.
Understanding location-specific symptoms
Lumbar (lower back) region
When a herniated disc occurs in the lumbar region, it can lead to pain that radiates from the lower back down into the buttocks, thighs, calves, and even the feet, a condition commonly known as sciatica. This type of pain often intensifies with activities such as sitting, standing, or driving for extended periods. The discomfort can be persistent, making it challenging to maintain regular activities without interruption.
Cervical (neck) region
The cervical region, located in the neck, can also be affected by a herniated disc. Here, the pain may manifest in the neck, shoulders, arms, or hands, often accompanied by tingling or weakness in the arm or fingers. Interestingly, pain in this area can sometimes mimic heart disease symptoms, especially if it radiates into the chest and arm, which can be alarming and confusing for those experiencing it.
Thoracic (mid back) region
Herniated discs in the thoracic region are less common but can present with vague and misleading symptoms. Pain might be felt in the upper or lower back, chest, abdomen, or even the legs. This variability in pain location can make diagnosis more challenging, as the symptoms might be mistaken for other conditions, such as gastrointestinal issues or cardiac problems.
Additional features and complications
Beyond the primary symptoms, herniated discs can also lead to muscle spasms, reduced reflexes, and difficulty with tasks requiring fine motor skills, such as holding objects. In severe cases, when nerve roots are extensively compressed, there can be a loss of bladder or bowel control, a condition known as cauda equina syndrome, which requires immediate medical attention.
Variability and silent herniated discs
It's crucial to understand that not everyone with a herniated disc will experience the same symptoms. In fact, some individuals may not notice any symptoms at all, with the condition only being discovered incidentally during imaging for other issues. This variability underscores the importance of comprehensive medical evaluation when symptoms do occur, as the absence of pain does not necessarily indicate the absence of a herniated disc.
The spectrum of symptoms associated with herniated discs is broad, and understanding the nuances of these sensations is essential for effective diagnosis and treatment. As we continue to explore this topic, we'll delve into real-world scenarios and patient experiences to further illustrate the impact of herniated discs on daily life and highlight when to seek medical attention.
Patient-centered perspectives on herniated discs
Understanding the real-world impact of a herniated disc involves delving into the daily experiences of those affected. Imagine waking up one morning to a sharp, burning pain shooting down your leg as you attempt to stand. This scenario is all too familiar for individuals with a herniated disc in the lumbar region, where the pain can be relentless and exacerbated by simple activities like sitting or bending.
In contrast, someone with a cervical herniated disc might find tasks such as typing or lifting objects challenging due to tingling and weakness in the hands or arms. The unpredictability of these symptoms can make planning daily activities difficult, often requiring adjustments to routines and sometimes leading to missed work or social engagements.
For those with thoracic herniations, the symptoms can be even more perplexing. A person might initially suspect a gastrointestinal issue when experiencing chest or abdominal discomfort, only to discover that the root cause is a herniated disc. These narratives underscore the importance of awareness and prompt medical evaluation to avoid prolonged discomfort and potential complications.
When to seek medical attention
Recognizing when to seek medical attention is crucial. Key indicators include the onset of new symptoms such as incontinence, severe muscle weakness, or persistent pain that disrupts daily life. These signs could indicate significant nerve compression and require immediate medical intervention. It's also essential to consult a healthcare provider if pain persists despite rest and over-the-counter medications, as early treatment can prevent further deterioration and improve outcomes.
Frequently asked questions
What are the common triggers for herniated disc symptoms?
Common triggers for herniated disc symptoms include activities that put pressure on the spine, such as heavy lifting, twisting motions, or even prolonged sitting. Coughing or sneezing can also exacerbate symptoms by increasing pressure on the affected nerves.
How can I differentiate herniated disc pain from other conditions?
Herniated disc pain often presents as sharp, radiating pain that follows the path of the affected nerve, such as sciatica for lumbar herniations. This is distinct from mechanical back pain, which is typically localized. Cervical herniations may mimic heart disease if the pain radiates into the chest and arm, but they are usually accompanied by tingling or weakness in the arm or fingers.
Can a herniated disc heal on its own?
In many cases, a herniated disc can heal over time with conservative treatments such as rest, physical therapy, and pain management. However, it's important to have a medical evaluation to rule out severe cases that might require more intensive interventions.
What treatments are available for a herniated disc?
Treatment options for a herniated disc vary based on the severity of symptoms. They include physical therapy to strengthen supportive muscles, medications for pain relief, and in some cases, surgical interventions to relieve nerve pressure. A healthcare provider can recommend the best approach based on individual needs and symptom severity.