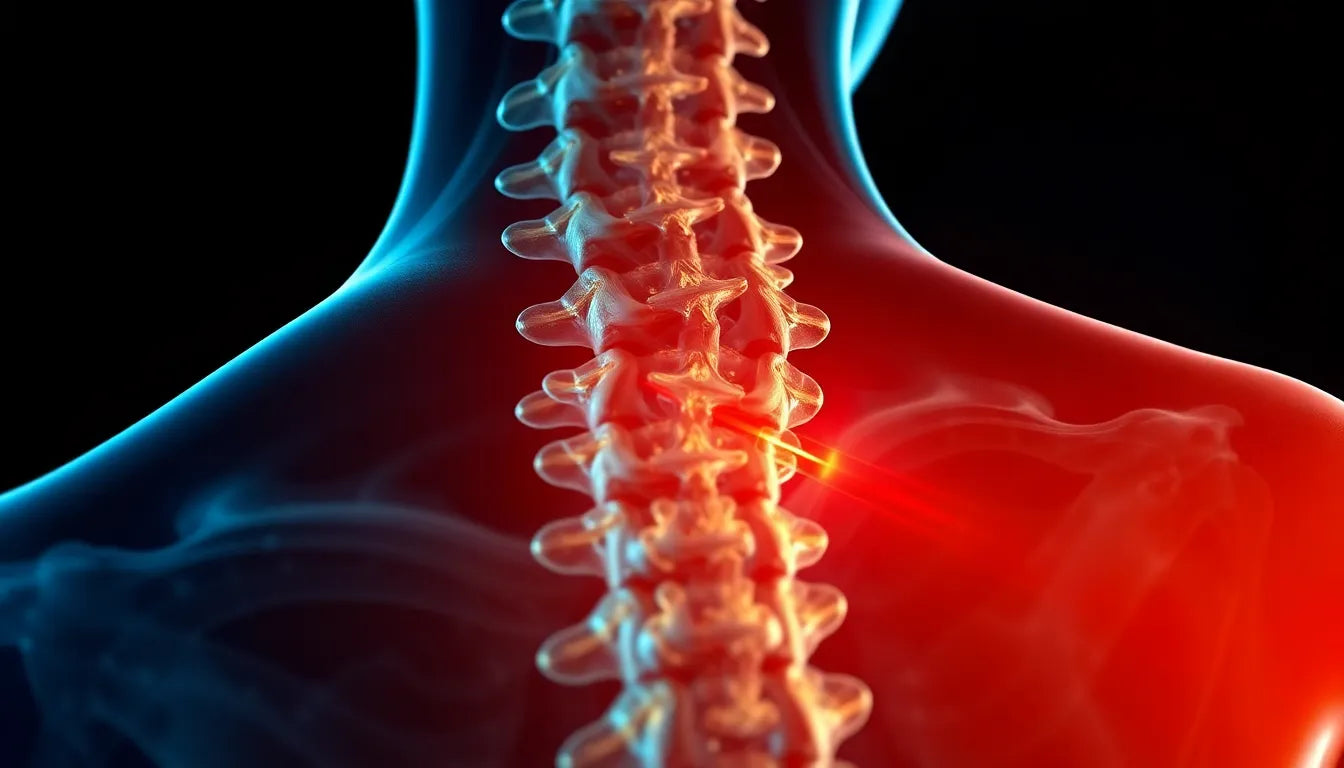
Understanding when a herniated disc requires surgical intervention is crucial for those experiencing this common spinal issue. A herniated disc occurs when the soft inner gel of a spinal disc pushes through a tear in its tougher outer layer. This can lead to nerve irritation and pain, affecting daily activities and overall quality of life. Herniated discs are surprisingly prevalent, particularly among adults aged 30 to 50, and can arise from various factors such as aging, injury, or improper lifting techniques.
Conservative treatments as the first line of defense
For most individuals, the good news is that herniated discs often improve without the need for surgery. Conservative treatments are typically the first step in managing this condition. Physical therapy, pain medications, and simply allowing time for healing can be incredibly effective. In fact, studies suggest that around 90% of patients experience significant improvement through non-surgical means. These treatments aim to alleviate pain, reduce inflammation, and restore normal function, allowing patients to return to their usual activities.
The role of surgery in herniated disc treatment
While conservative treatments are successful for the majority, there are specific scenarios where surgery becomes a necessary consideration. Understanding when to opt for surgical intervention is essential for making informed decisions about one's health. Surgery may be required when symptoms persist despite exhaustive non-surgical efforts or when certain severe symptoms manifest. Recognizing these situations can help patients and healthcare providers make timely and appropriate decisions regarding surgical options.
In the following sections, we will explore the critical indications for surgery, the various surgical procedures available, and the decision-making process that involves both patients and healthcare providers. By understanding these factors, individuals can better navigate their treatment options and make choices that align with their health goals and lifestyle needs.
When surgery becomes essential for herniated discs
Determining when surgery is necessary for a herniated disc involves understanding both absolute and relative indications. Absolute indications are scenarios where surgery is imperative to prevent further damage or address critical symptoms. These include progressive or severe neurological deficits, such as noticeable leg weakness or numbness, and myelopathy, which involves symptoms of spinal cord compression. One of the most urgent conditions requiring immediate surgical intervention is cauda equina syndrome. This condition is marked by the loss of bowel or bladder control, saddle anesthesia, or severe weakness, and is considered a surgical emergency.
Evaluating discretionary indications for surgery
In addition to absolute indications, there are relative or discretionary scenarios where surgery might be considered based on individual circumstances. Persistent, severe pain that significantly impairs daily activities and quality of life is a key factor. If such pain does not respond to at least six weeks of conservative care, surgery may be an option. Furthermore, a lack of improvement after a reasonable course of non-surgical management can lead healthcare providers to consider surgical intervention. For cervical disc issues, symptoms persisting over six months without response to treatment may also warrant surgical consideration.
Understanding surgical procedures for herniated discs
When surgery is deemed necessary, several surgical options are available, each with its specific purpose and approach. A discectomy, including microdiscectomy, involves the removal of herniated disc material to relieve nerve pressure. This procedure is often chosen for its effectiveness in alleviating pain and restoring function. Another option is a laminotomy or laminectomy, where part or all of the vertebral bone (lamina) is removed to access and relieve pressure on spinal nerves. In cases requiring stabilization post-disc removal, spinal fusion is performed to secure the spine. Additionally, artificial disc replacement is selectively used under favorable conditions, offering an alternative to fusion by maintaining more natural spinal movement.
Decision-making process: patient and provider collaboration
The decision to proceed with surgery involves a collaborative process between patients and healthcare providers. It is crucial to consider the severity and duration of symptoms, response to previous treatments, and the patient's overall health and lifestyle preferences. Shared decision-making ensures that patients are fully informed about the potential risks and benefits of surgical interventions, allowing them to make choices that best align with their personal health goals. This collaborative approach not only empowers patients but also enhances the likelihood of successful outcomes.
As we delve deeper into the nuances of surgical options and the decision-making process, it becomes evident that surgery for herniated discs is a highly individualized choice. By understanding the absolute and relative indications for surgery, the various procedures available, and the importance of patient-provider collaboration, individuals can navigate their treatment options with confidence and clarity. This comprehensive understanding is key to making informed decisions that promote long-term health and well-being.
Long-term outcomes and considerations
For many individuals with herniated discs, the long-term outcomes of surgical and non-surgical treatments can be quite similar. While surgery may provide quicker relief from severe symptoms, non-surgical approaches such as physical therapy and lifestyle modifications often lead to substantial improvement over time. It is important to weigh these outcomes when considering surgery, as the potential risks and benefits must be carefully evaluated.
Surgical interventions, while effective in specific cases, come with inherent risks such as infection, nerve damage, and the possibility of needing additional surgeries in the future. Patients must discuss these risks with their healthcare providers to understand how they might impact their personal health situation. Ultimately, the decision to undergo surgery should be based on a comprehensive understanding of both the immediate and long-term implications.
Real patient stories and testimonials
Many patients who have experienced herniated discs share diverse stories of recovery and treatment. For instance, John, a 45-year-old office worker, opted for a microdiscectomy after several months of debilitating pain that did not improve with physical therapy. Post-surgery, he reported significant relief and a return to his normal activities within a few weeks. Conversely, Lisa, a 50-year-old teacher, chose to manage her symptoms through a combination of physical therapy and lifestyle changes. Over time, she experienced a gradual reduction in pain and improved mobility without the need for surgery.
These testimonials highlight the varied paths to recovery and emphasize the importance of personalized treatment plans. Each patient’s journey is unique, and what works for one individual may not be suitable for another. Therefore, it is crucial for patients to work closely with their healthcare providers to determine the best approach for their specific condition.
Frequently asked questions
What are the risks of herniated disc surgery?
Herniated disc surgery, like any surgical procedure, carries certain risks. These include infection, nerve damage, blood clots, and the potential for additional surgeries if the initial procedure does not fully resolve the issue. Discussing these risks with a healthcare provider is essential to making an informed decision about surgery.
How long is the recovery period after herniated disc surgery?
The recovery period can vary depending on the type of surgery and the individual’s overall health. Generally, patients may return to light activities within a few weeks, but full recovery can take several months. Factors such as adherence to post-operative care instructions and participation in rehabilitation can influence recovery speed.
Can lifestyle changes prevent the need for surgery?
Lifestyle changes, such as regular exercise, maintaining a healthy weight, and practicing proper body mechanics, can help manage herniated disc symptoms and potentially prevent the need for surgery. These modifications can reduce stress on the spine and improve overall spinal health.
How can I tell if my symptoms are severe enough to consider surgery?
Symptoms that may warrant surgical consideration include persistent, severe pain that significantly impairs daily activities, progressive neurological deficits, or emergency symptoms like loss of bowel or bladder control. It is important to consult a healthcare provider to evaluate the severity of symptoms and determine the appropriate course of action.
Is there a difference in outcomes between open and minimally invasive surgery?
Minimally invasive surgery often results in shorter recovery times and less postoperative pain compared to open surgery. However, the choice between these approaches depends on the specific case and the surgeon’s expertise. Both methods aim to relieve pressure on the affected nerves, but the recovery experience and outcomes may vary.
Sources
- WebMD. "When Do I Need Surgery for a Herniated Disk?"
- Twin Cities Orthopedics. "Spine Surgeon’s Guide to Herniated Discs."
- PubMed. "Herniated discs: when is surgery necessary?"
- Orthobullets. "Lumbar Disc Herniation."
- American Association of Neurological Surgeons (AANS). "Herniated Disc."
- MyHealth Alberta. "Lumbar Herniated Disc: Should I Have Surgery?"