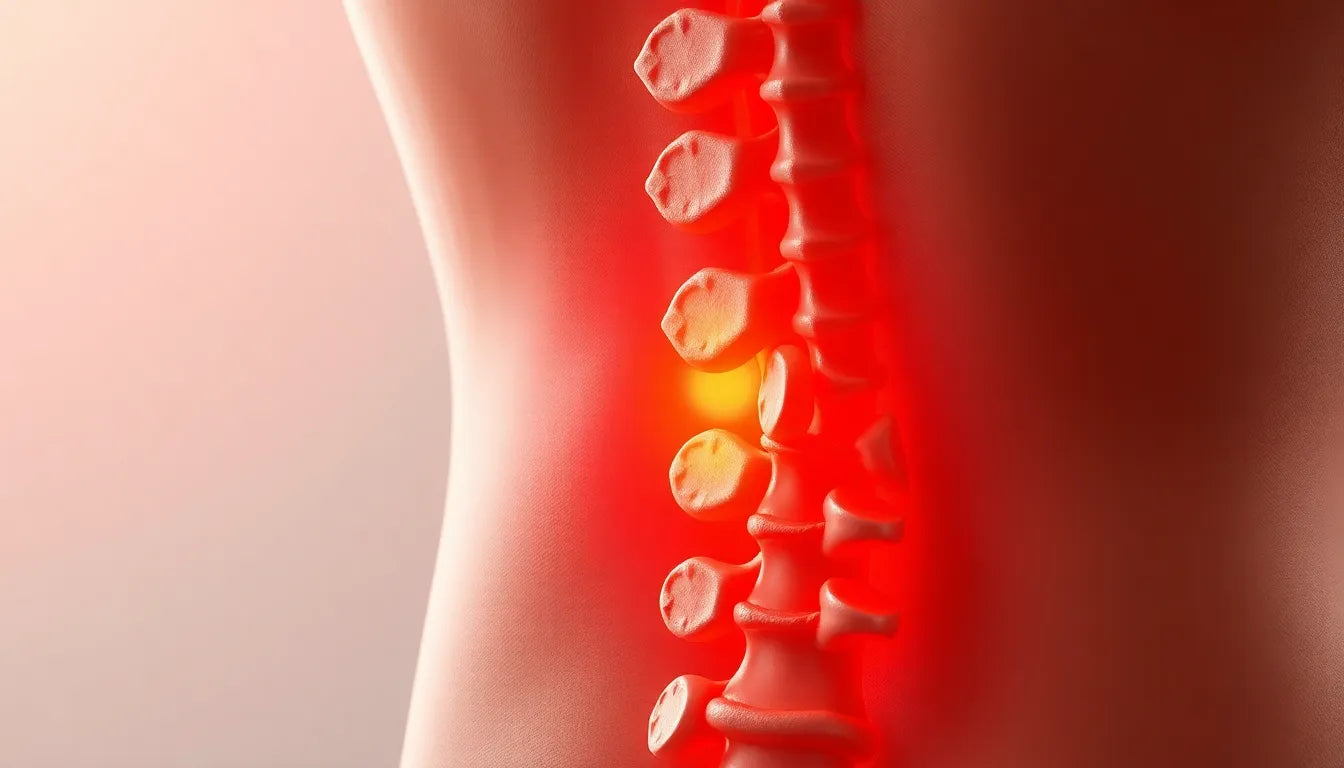
Understanding the treatment of a herniated disc begins with recognizing what a herniated disc actually is. A herniated disc occurs when the soft inner gel of an intervertebral disc pushes through a tear in the tougher exterior, often resulting in pain and discomfort. This condition can be triggered by various factors, including aging, improper lifting techniques, or even sudden trauma. Common symptoms of a herniated disc include sharp pain, numbness, and weakness in the limbs, which can significantly disrupt daily activities and overall quality of life.
the importance of timely treatment
Addressing a herniated disc promptly is crucial to prevent further complications, such as chronic pain or nerve damage. Timely intervention not only alleviates symptoms but also helps in maintaining mobility and preventing long-term disability. Treatment approaches for herniated discs can vary widely, ranging from conservative methods like physical therapy and medication to more invasive surgical options. The choice of treatment depends on the severity of the condition and the specific needs of the patient.
setting the stage for relief
For those suffering from a herniated disc, the journey to relief can seem daunting. However, understanding the array of treatment options available can provide hope and direction. From non-invasive therapies that focus on strengthening and pain management to advanced surgical techniques, there are numerous ways to address this condition effectively. In the following sections, we will delve into these options, offering insights that can help you regain control over your life and improve your overall well-being. Whether you're exploring conservative treatments or considering surgical interventions, the right approach can lead to significant improvements and a return to a more active lifestyle.
conservative treatments for herniated discs
When it comes to treating a herniated disc, many patients find relief through conservative treatments, which are often effective for managing symptoms and improving function. One of the primary approaches is physical therapy. This involves exercises specifically designed to strengthen the core and back muscles, which support the spine and help reduce pressure on the herniated disc. Physical therapists can tailor a program to each individual's needs, focusing on improving flexibility and stability, which are crucial for reducing pain and preventing further injury.
Another cornerstone of conservative treatment is pain management. This can include both over-the-counter medications like ibuprofen or acetaminophen and prescription drugs for more severe pain. Muscle relaxants and anti-inflammatory medications are also commonly used to alleviate discomfort and decrease inflammation around the affected area.
Activity modification is an equally important aspect of conservative treatment. Patients are advised to avoid movements that exacerbate their symptoms. This might involve altering how they sit, stand, or lift objects to minimize strain on the back. Simple adjustments, such as maintaining a neutral spine posture and using ergonomic aids, can significantly reduce pain and facilitate recovery.
In addition to these methods, hot and cold therapy offers a non-invasive way to manage symptoms. Cold therapy, such as ice packs, can help reduce inflammation and numb acute pain, while heat therapy, like warm compresses, can enhance blood flow and promote healing by relaxing tense muscles.
minimally invasive interventions
For those who do not find sufficient relief from conservative treatments, minimally invasive interventions can be an effective next step. Spinal injections, such as epidural steroid injections and nerve blocks, are commonly used to provide temporary relief by reducing inflammation around the affected nerves. These injections can help decrease pain and improve mobility, making it easier for patients to participate in physical therapy and other activities.
Another minimally invasive technique is spinal decompression. This non-surgical procedure involves gently stretching the spine to change its position, which can help reposition the herniated disc and relieve pressure on the nerves. This method can be particularly beneficial for those who experience significant nerve-related pain.
Additionally, alternative therapies such as acupuncture, chiropractic care, and massage therapy can complement conventional treatments. Acupuncture may help alleviate pain by stimulating specific points on the body, while chiropractic adjustments focus on realigning the spine to reduce pressure on the nerves. Massage therapy can help relax muscles and improve circulation, contributing to overall pain relief and recovery.
By exploring these various treatment options, individuals suffering from a herniated disc can find a combination of therapies that work best for their specific condition, paving the way for improved quality of life and a return to normal activities.
Exploring surgical options for herniated discs
When conservative and minimally invasive treatments do not provide adequate relief, surgical interventions may be considered for treating a herniated disc. One of the most common surgical procedures is microdiscectomy. This technique is often referred to as the "gold standard" for herniated disc surgery. During a microdiscectomy, a small portion of the herniated disc is removed to relieve pressure on the affected nerve. Patients typically experience significant pain relief and improved mobility following the procedure. Recovery times can vary, but many individuals return to normal activities within a few weeks, with physical therapy often recommended to aid in the recovery process.
In cases of spinal instability or recurrent herniations, spinal fusion may be the preferred surgical option. This procedure involves joining two or more vertebrae together to stabilize the spine and prevent further movement that could cause pain. While spinal fusion can lead to long-term stability and pain relief, it may also reduce spinal flexibility. Patients considering this option should discuss the potential benefits and drawbacks with their healthcare provider to determine if it aligns with their lifestyle and recovery goals.
Another surgical alternative is artificial disc replacement. This procedure involves replacing the damaged disc with an artificial one made from metal and plastic. Unlike spinal fusion, artificial disc replacement aims to maintain spinal motion while alleviating pain. This option can be beneficial for younger patients or those seeking to preserve spinal flexibility. However, it is essential to weigh the pros and cons with a medical professional, as not all patients are suitable candidates for this type of surgery.
Conclusion
Understanding the diverse treatment options for a herniated disc is crucial for finding the most effective path to relief. Whether through conservative, minimally invasive, or surgical methods, a tailored approach can significantly improve quality of life. It is essential for patients to consult healthcare professionals to develop a personalized treatment plan that addresses their specific needs and goals. By exploring all available options, individuals can take proactive steps toward recovery and regain control over their daily activities.
Frequently Asked Questions
What is the success rate of conservative treatments for herniated discs?
Conservative treatments, such as physical therapy and pain management, have a high success rate for many individuals, particularly when the herniated disc is not severely compressing nerves. Success stories often involve significant pain reduction and improved function, allowing patients to return to normal activities without the need for surgery.
How long does it take to recover from a herniated disc surgery?
Recovery times from herniated disc surgery vary depending on the type of procedure and the patient's overall health. Generally, patients can expect to return to normal activities within 4 to 6 weeks after a microdiscectomy, while recovery from spinal fusion or artificial disc replacement may take several months. Factors such as adherence to physical therapy and lifestyle modifications can also influence recovery duration.
Are there any lifestyle changes that can prevent future herniated discs?
Yes, adopting certain lifestyle changes can help prevent future herniated discs. These include maintaining a healthy weight, practicing good posture, engaging in regular physical activity to strengthen core muscles, and using proper techniques when lifting heavy objects. Ergonomic aids can also support spinal health and reduce the risk of recurrence.
Can ergonomic aids really help in managing herniated disc symptoms?
Ergonomic aids, such as supportive chairs, lumbar cushions, and standing desks, can play a significant role in managing herniated disc symptoms. These tools help maintain proper posture, reduce strain on the spine, and promote a comfortable and supportive environment, aiding in both recovery and prevention of future issues.
Is alternative therapy effective for herniated discs?
Alternative therapies, including acupuncture, chiropractic care, and massage therapy, can be effective in complementing conventional treatments for herniated discs. While these therapies may not replace medical treatments, they can provide additional pain relief and relaxation, contributing to overall recovery and well-being. It is advisable to discuss these options with a healthcare provider to ensure they are suitable for your specific condition.
Sources
- Mayo Clinic. "Herniated disk - Diagnosis and treatment."
- Cleveland Clinic. "Herniated Disk (Slipped or Bulging Disk)."
- Sciatica.com. "11 Treatment Options for Herniated Discs."
- WebMD. "Herniated Disk Treatment, Remedies, and Medications."
- Spine-health. "Treatment for a Lumbar Herniated Disc."
- University of Rochester Medical Center. "Herniated Disc | Conditions & Treatments."
- Northeast Spine and Sports. "What Is the Best Treatment for a Herniated Disc?"