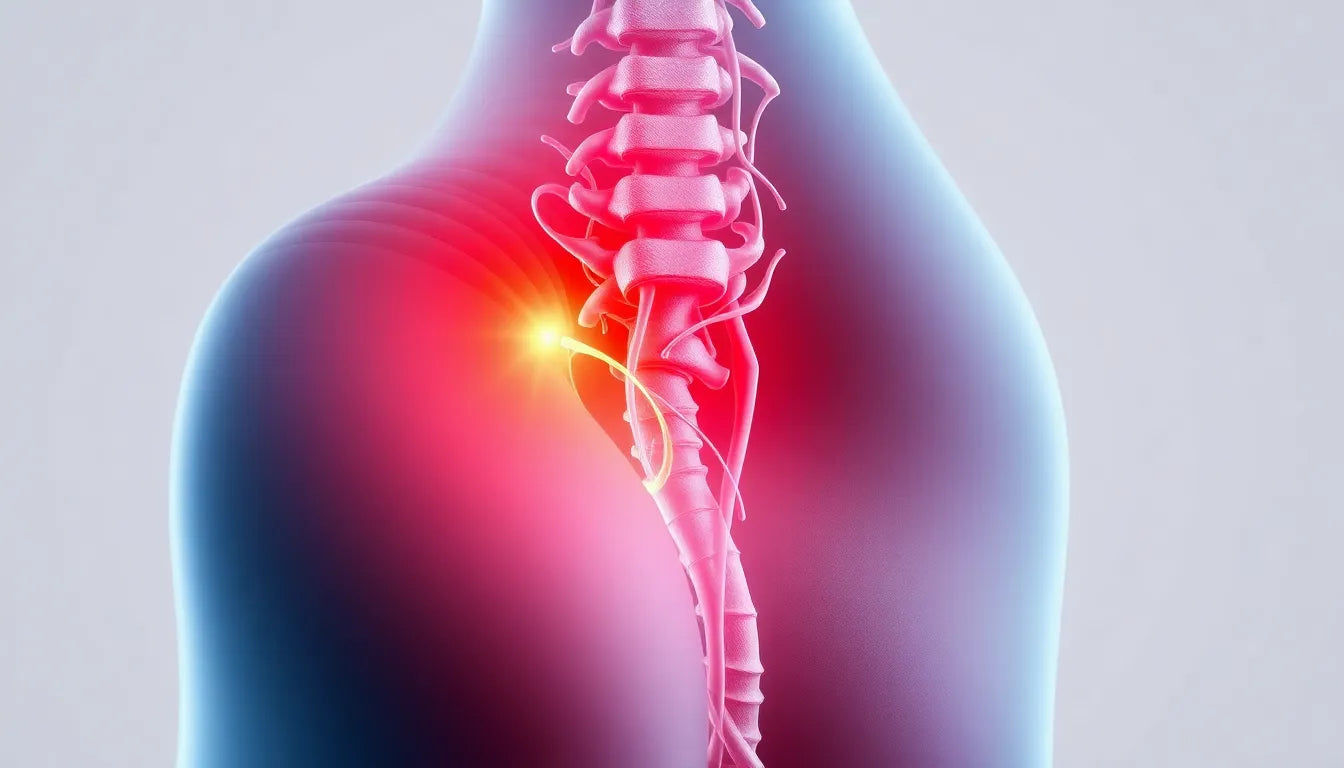
Understanding the sensations associated with a herniated disc is crucial for anyone experiencing back pain or discomfort. A herniated disc, also known as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a crack in its tougher exterior. This condition can result in significant pain and discomfort, impacting daily activities and overall quality of life. Recognizing the symptoms early is essential for managing pain effectively and preventing further complications.
Understanding herniated discs
A herniated disc typically develops due to wear and tear, known as disc degeneration, or from an injury. The spine is composed of a series of bones (vertebrae) cushioned by discs that act as shock absorbers. When a disc herniates, its inner gel-like core leaks out, potentially pressing on nearby nerves. This pressure can lead to a range of symptoms, depending on the location of the herniation within the spine.
It's important to note that symptoms of a herniated disc can vary widely. The location of the herniation plays a significant role in determining the type and severity of pain experienced. For instance, a herniation in the lumbar region (lower back) may cause different sensations compared to one in the cervical region (neck). Understanding these variations is key to identifying the condition accurately.
The significance of symptom awareness
Herniated discs are a common occurrence, affecting many individuals at some point in their lives. Despite their prevalence, the impact on daily life can be profound, with symptoms ranging from mild discomfort to debilitating pain. This makes it crucial for individuals to be aware of the specific symptoms associated with herniated discs, as accurate identification can help differentiate this condition from other types of back issues.
Being aware of the symptoms not only aids in seeking appropriate medical attention but also helps in implementing effective management strategies. Early identification can lead to better outcomes, allowing individuals to maintain their quality of life and avoid unnecessary complications. By understanding what a herniated disc feels like, individuals can take proactive steps towards addressing their symptoms and exploring potential treatment options.
In the following sections, we will delve deeper into the specific sensations associated with herniated discs, exploring how pain characteristics and associated symptoms differ based on the location of the herniation. This knowledge will empower readers to better understand their condition and make informed decisions about their health and well-being.
pain characteristics and location
Understanding the specific sensations that accompany a herniated disc is essential for identifying the condition and seeking appropriate treatment. The pain experienced can vary significantly depending on the location of the herniation within the spine. Each region of the spine—lumbar, cervical, and thoracic—presents its own unique set of symptoms and challenges.
lumbar herniation
When a herniated disc occurs in the lumbar region, or lower back, it often results in sciatic pain. This type of pain is typically described as sharp, burning, or stinging, and it radiates from the buttocks down one leg, following the path of the sciatic nerve. This can lead to significant discomfort, making it difficult to perform everyday activities such as walking or sitting for extended periods.
cervical herniation
In the cervical region, or neck, a herniated disc can cause pain that radiates between the shoulder blades and down the arms into the hands. This pain may be accompanied by a reduction in neck mobility, making it challenging to turn the head or hold the neck in certain positions. These symptoms can interfere with tasks that require arm and hand movement, such as typing or lifting objects.
thoracic herniation
Though less common, a herniated disc in the thoracic region, or mid-back, can cause pain that radiates around the rib cage to the chest or abdomen. This type of herniation can be particularly challenging to diagnose due to the overlap of symptoms with other conditions that affect the chest and abdomen. However, understanding this pain pattern can help differentiate it from other potential causes.
associated symptoms
In addition to pain, herniated discs can produce a variety of other symptoms that can impact daily life. These associated symptoms provide further clues about the nature and severity of the condition.
muscle weakness
A herniated disc can lead to muscle weakness in the areas served by the affected nerves. This weakness can manifest as difficulty walking, maintaining balance, or gripping objects firmly. Such symptoms can severely limit a person's ability to carry out routine tasks and may increase the risk of falls or injuries.
numbness and tingling
Numbness or tingling sensations often accompany herniated discs, occurring in the areas innervated by the compressed nerves. These sensations can be intermittent or persistent, and they may affect the hands, arms, legs, or feet, depending on the location of the herniation.
muscle spasms
Muscle spasms are another common symptom, occurring in the back or neck region. These involuntary contractions can be painful and may further restrict movement, compounding the discomfort caused by the herniated disc.
pain aggravated by movement
Certain movements, such as coughing, sneezing, or bending, can exacerbate the pain associated with a herniated disc. This is due to the increased pressure placed on the affected nerves during these actions, which can intensify the pain and discomfort.
reduced reflexes
In cases of lumbar herniation, individuals may experience reduced reflexes, particularly in the knee or ankle. This can be a subtle yet important sign of nerve involvement and should be evaluated by a healthcare professional to determine the extent of the nerve compression.
By understanding these pain characteristics and associated symptoms, individuals can better recognize the signs of a herniated disc and seek timely medical attention. In the next section, we will explore severe symptoms that require immediate medical intervention and discuss strategies for managing symptoms effectively.
Severe symptoms requiring immediate attention
While many symptoms of a herniated disc can be managed conservatively, certain severe symptoms require immediate medical attention to prevent long-term complications. Recognizing these red flag symptoms is crucial for ensuring timely intervention and care.
Red flag symptoms
Some symptoms indicate a more serious issue and necessitate urgent medical evaluation. These include:
- Loss of bowel or bladder control: This can signify a condition known as cauda equina syndrome, which requires immediate medical intervention.
- Numbness around the genital area, buttocks, or backs of thighs: Known as saddle anesthesia, this is another potential sign of cauda equina syndrome.
- Increasing difficulty with balance and coordination: This may indicate significant nerve involvement and requires prompt assessment by a healthcare professional.
These symptoms suggest that the herniated disc may be compressing critical nerves, and delaying treatment could lead to permanent damage.
Symptom progression and management
The symptoms of a herniated disc can evolve over time, starting with mild discomfort and potentially progressing to severe pain and neurological deficits. Early intervention and management are key to preventing this progression and maintaining quality of life.
Ergonomic considerations
Implementing ergonomic adjustments in daily activities can significantly alleviate symptoms and prevent further injury. Anodyne offers a range of products designed to support spinal health, including ergonomic chairs and cushions that promote proper posture and reduce strain on the spine.
Incorporating these products into your daily routine can help manage pain and improve comfort, especially for those who spend long hours sitting or performing repetitive tasks.
Frequently asked questions
What are the early signs of a herniated disc?
Early signs of a herniated disc often include localized pain in the back or neck, stiffness, and discomfort that worsens with movement. These initial symptoms can serve as a warning to seek medical evaluation before the condition progresses.
How can I differentiate herniated disc pain from other back pain?
Herniated disc pain is often characterized by sharp, burning, or stinging sensations that radiate along specific nerve paths, such as down the leg or arm. Unlike general back pain, which may be more diffuse, herniated disc pain is usually more intense and follows a distinct pattern.
When should I consult a doctor for herniated disc symptoms?
Consult a doctor if you experience persistent pain, numbness, or weakness that interferes with daily activities, or if you notice any red flag symptoms such as loss of bowel or bladder control. Early consultation can help prevent complications and guide appropriate treatment.
Are there non-surgical treatments for herniated discs?
Yes, non-surgical treatments include physical therapy, pain management medications, and lifestyle modifications. Ergonomic adjustments and exercises designed to strengthen the back and improve flexibility are also effective in managing symptoms.
Can lifestyle changes help manage herniated disc symptoms?
Absolutely. Maintaining good posture, engaging in regular low-impact exercise, and using ergonomic supports can significantly reduce symptoms. These lifestyle changes can help minimize stress on the spine and promote overall spinal health.
By understanding the symptoms and management strategies for herniated discs, individuals can take proactive steps to address their condition and improve their quality of life. Early recognition and intervention are key to managing this common spinal issue effectively.
Sources
- Cleveland Clinic. "Herniated Disk."
- NCBI StatPearls. "Lumbar Disc Herniation."
- American Association of Neurological Surgeons. "Herniated Disc."
- NewYork-Presbyterian. "Herniated Disc: Symptoms and Treatments."
- Main Line Spine. "Herniated Disc."
- Harvard Health. "Herniated Disk in the Lumbar Spine."
- Johns Hopkins Medicine. "Lumbar Disk Disease (Herniated Disk)."