A herniated disc in the lower back is a common condition that can significantly impact an individual's quality of life. This condition occurs when the soft, gel-like center of a spinal disc pushes through a tear in the tougher exterior casing, often affecting the lumbar region of the spine. As a prevalent issue, understanding how a herniated disc feels and recognizing its symptoms are crucial for early diagnosis and effective treatment.
understanding the importance of symptom recognition
Identifying the symptoms of a herniated disc is vital because it allows for timely medical intervention, which can prevent further complications and promote recovery. The symptoms can vary widely but typically include pain, discomfort, and a range of sensations that can interfere with daily activities. Recognizing these signs early can lead to more effective management and a quicker return to normal life.
personal impact on daily life
The symptoms of a herniated disc in the lower back can profoundly affect daily life, influencing everything from mobility to overall comfort. Individuals may experience pain that limits their ability to perform routine tasks, such as bending, lifting, or even sitting for extended periods. This can lead to a decrease in productivity and enjoyment of activities, emphasizing the importance of understanding and addressing the condition's impact.
As we delve deeper into this topic, we will explore the specific sensations and symptoms associated with a herniated disc in the lower back, providing a comprehensive overview of what sufferers may experience. This understanding is not only beneficial for those currently affected but also for anyone seeking to prevent or mitigate the effects of this common spinal issue.
detailed symptoms of a herniated disc in the lower back
Experiencing a herniated disc in the lower back can manifest through a variety of symptoms, each with its own impact on daily life. The most common symptom is back pain, which can range from a dull ache to sharp, intense pain. This pain may be intermittent or continuous, often worsening with specific movements such as bending, lifting, or even simple actions like coughing or sneezing. The intensity and duration of the pain can vary greatly, making it a challenging condition to manage.
sciatica: a common companion
One of the hallmark symptoms associated with a herniated disc in the lower back is sciatica. This condition is characterized by sharp or shooting pain that radiates from the lower back down through the buttocks and into the legs and feet. The pain can significantly affect mobility, making it difficult to walk, stand, or even sit comfortably. This radiating pain is due to the pressure the herniated disc places on the sciatic nerve, one of the largest nerves in the body.
muscle spasms and weakness
In addition to pain, individuals with a herniated disc may experience muscle spasms in the back. These involuntary contractions can be painful and may lead to further discomfort and stiffness. Muscle weakness, particularly in the legs, is another symptom that can arise from nerve compression. This weakness can affect balance and strength, increasing the risk of falls and making everyday tasks more challenging.
numbness and tingling sensations
Numbness and tingling in the legs and feet are also common symptoms of a herniated disc. These sensations are often indicative of nerve involvement and can range from mild tingling to complete numbness. Such symptoms can disrupt normal sensory perception, making it difficult to gauge temperature or pressure, which can be particularly concerning when walking or performing other activities.
changes in reflexes
Another neurological symptom that may accompany a herniated disc is a change in reflexes, particularly at the knee or ankle. Decreased reflex responses can be a sign of nerve dysfunction, further highlighting the impact of the herniated disc on the nervous system. These changes can affect coordination and movement, complicating simple actions like walking or climbing stairs.
understanding the anatomy and progression of herniation
The lumbar spine, located in the lower back, consists of vertebrae separated by intervertebral discs. These discs act as cushions, absorbing shock and allowing for flexibility. A herniated disc occurs when the inner gel-like core of a disc protrudes through a tear in its outer layer. This process can happen gradually or suddenly and is often categorized into stages, from initial bulging to complete herniation.
In the early stages, symptoms may be mild and easily overlooked. However, as the herniation progresses, the symptoms typically become more pronounced. Understanding these stages is crucial for recognizing the condition early and seeking appropriate treatment to prevent further deterioration.
impact on daily activities
The symptoms of a herniated disc can severely impact daily activities. Sitting for prolonged periods, such as at a desk or in a car, can exacerbate pain and discomfort. Similarly, standing for extended durations can also trigger or worsen symptoms. These limitations can lead to significant lifestyle adjustments, affecting work performance and social interactions.
Mobility challenges are another major concern. Walking, climbing stairs, or even simple tasks like bending to tie shoes can become painful and laborious. These challenges highlight the need for effective management strategies to maintain a good quality of life despite the condition.
Understanding the detailed symptoms and their impact on daily life is essential for those affected by a herniated disc in the lower back. By recognizing these signs and seeking timely medical advice, individuals can better manage their condition and work towards recovery.
Diagnosis and medical evaluation for a herniated disc
Diagnosing a herniated disc in the lower back involves a combination of medical history, physical examination, and imaging tests. Medical professionals typically begin by reviewing the patient's symptoms and medical history to identify patterns that suggest a herniated disc. A physical examination is then conducted to assess nerve function, muscle strength, and reflexes. This helps in pinpointing the affected area and evaluating the extent of nerve involvement.
Imaging tests, such as MRI (Magnetic Resonance Imaging), are crucial in confirming the diagnosis. An MRI provides detailed images of the spine's soft tissues, allowing doctors to see the exact location of the herniated disc and the degree of herniation. In some cases, a CT scan or X-ray may be used to rule out other conditions. These diagnostic tools are essential for developing an effective treatment plan tailored to the individual's needs.
Consultation with healthcare professionals
Consulting with healthcare professionals is a vital step in managing a herniated disc. A specialist, such as an orthopedic doctor or neurologist, can provide a comprehensive evaluation and recommend appropriate treatment options. This may include physical therapy, pain management strategies, and in severe cases, surgical intervention. Early consultation can prevent the condition from worsening and promote recovery, enabling individuals to maintain a better quality of life.
Personal experiences and case studies
Hearing personal experiences from those who have dealt with a herniated disc can offer valuable insights and reassurance. For instance, Jane, a 45-year-old office worker, shared how she initially ignored her back pain until it became debilitating. After consulting a specialist and undergoing physical therapy, she learned to manage her symptoms effectively, allowing her to return to her daily activities with minimal discomfort.
Case studies like Jane's highlight the importance of early diagnosis and intervention. They also demonstrate how personalized treatment plans can lead to successful management of the condition, emphasizing the role of professional guidance and patient commitment in the recovery process.
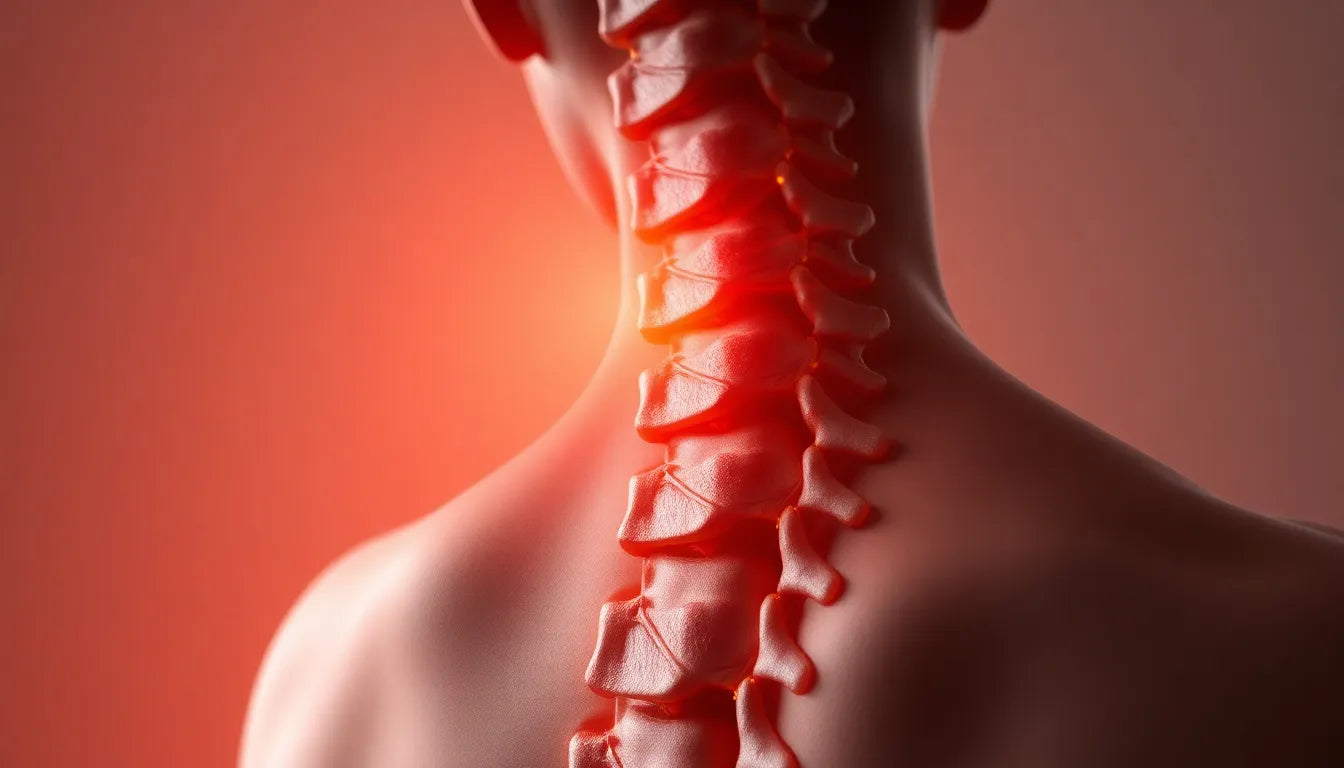
Visual aids for understanding herniated discs
Visual aids, such as diagrams and infographics, can significantly enhance the understanding of a herniated disc's anatomy and symptoms. These tools provide a clear representation of the lumbar spine structure, showing how the discs are positioned between the vertebrae and illustrating the process of herniation. Visual content can make complex medical information more accessible, helping individuals grasp the condition's impact and the importance of seeking treatment.
Frequently asked questions
What are the stages of a herniated disc?
The progression of a herniated disc typically begins with a disc bulge, where the outer layer of the disc weakens but remains intact. This can progress to a protrusion, where the inner gel-like material starts to push through. In the extrusion stage, the material breaks through the outer layer but remains connected to the disc. Finally, in the sequestration stage, the material separates entirely and can move into the spinal canal. Recovery can vary depending on the stage and treatment received.
How is a herniated disc diagnosed?
A herniated disc is diagnosed through a combination of medical history review, physical examination, and imaging tests. Doctors assess symptoms and perform tests to evaluate nerve function and reflexes. Imaging tests like MRI or CT scans provide detailed views of the spine, confirming the presence and extent of herniation.
Can a herniated disc heal on its own?
In some cases, a herniated disc can heal on its own, particularly if the herniation is mild. The body can reabsorb the extruded material over time, reducing pressure on the nerves. Factors such as age, overall health, and adherence to treatment plans can influence recovery. However, medical intervention is recommended if symptoms persist or worsen.
What treatment options are available?
Treatment for a herniated disc may include physical therapy, which focuses on exercises to strengthen the back and improve flexibility. Pain management options, such as anti-inflammatory medications or corticosteroid injections, can alleviate discomfort. In severe cases, surgical intervention, such as a discectomy, may be necessary to remove the herniated portion of the disc.
How can lifestyle changes help manage symptoms?
Lifestyle changes can play a crucial role in managing herniated disc symptoms. Regular exercise, maintaining a healthy weight, and practicing good posture can alleviate pressure on the spine. Ergonomic adjustments at work and home, such as using supportive chairs and avoiding prolonged sitting, can also help reduce discomfort and prevent further injury.