Back pain is a widespread issue that affects millions of people around the globe, often disrupting daily life and diminishing quality of living. While back pain can result from various causes, one of the more serious and common culprits is a herniated disc. Understanding what a herniated disc is and recognizing its signs early on can be crucial for effective management and treatment, potentially preventing long-term complications.
Understanding the anatomy of the spine
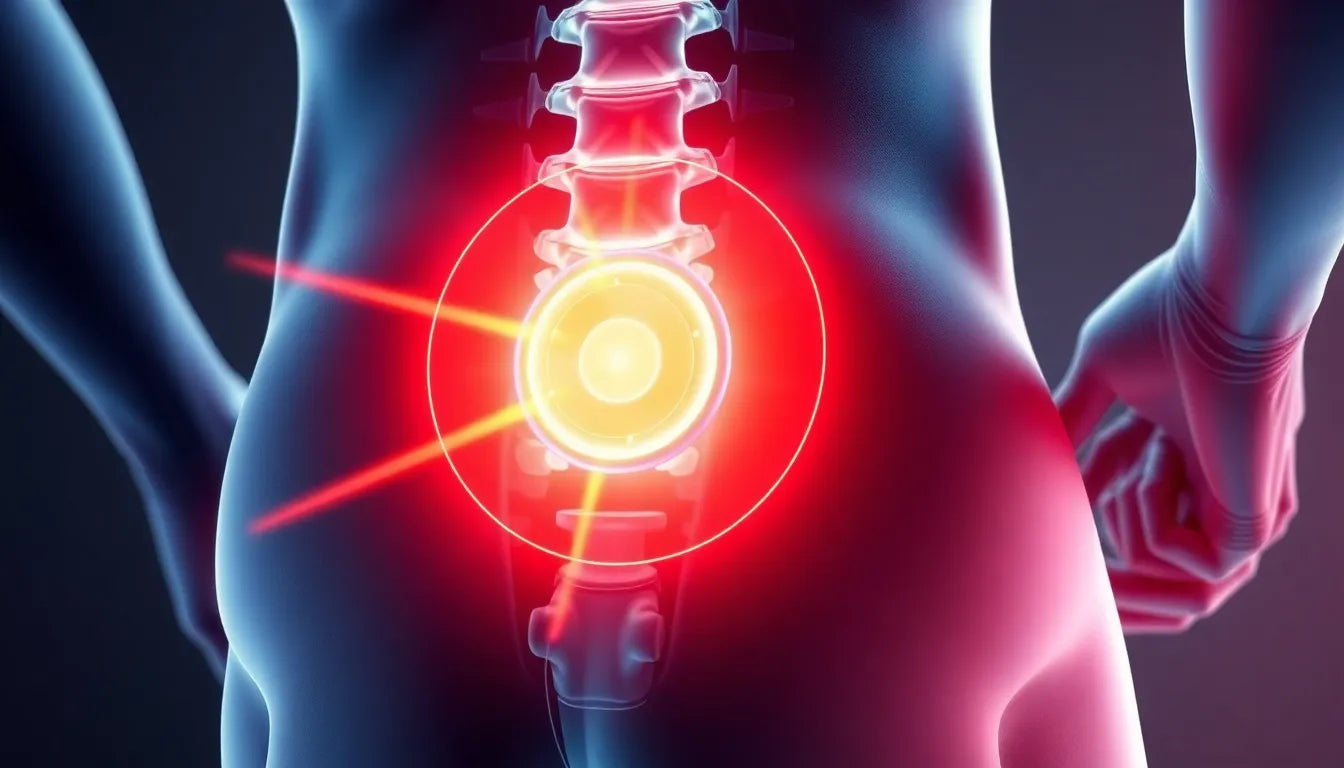
The spine is a complex structure composed of vertebrae, intervertebral discs, nerves, and other tissues that work together to support the body and allow for movement. Discs act as cushions between the vertebrae, absorbing shocks and providing flexibility to the spine. A herniated disc, sometimes referred to as a slipped or ruptured disc, occurs when the soft inner core of a disc protrudes through its tougher outer layer. This condition can lead to irritation or compression of nearby nerves, resulting in pain and other symptoms.
Why accurate diagnosis matters
Distinguishing a herniated disc from other types of back pain is essential for several reasons. First, it allows for targeted treatment that addresses the specific cause of the pain. Misdiagnosis can lead to ineffective treatment plans and prolonged discomfort. Furthermore, untreated herniated discs can lead to chronic pain, nerve damage, and even loss of mobility. Therefore, understanding the symptoms and seeking a professional diagnosis can significantly improve outcomes and quality of life.
By being informed about the signs and symptoms of a herniated disc, individuals can take proactive steps in seeking medical advice and exploring treatment options. Early intervention can mitigate pain, improve recovery times, and prevent further complications, highlighting the importance of awareness and education on this common spinal issue.
common symptoms of a herniated disc
Identifying the symptoms of a herniated disc is crucial for determining whether your back pain requires professional attention. Often, the location of the herniated disc within the spine will dictate the specific symptoms experienced. Commonly, individuals with a herniated disc report pain concentrated in the lower back or neck, depending on the affected region of the spine. This pain can range from a dull ache to sharp, intense discomfort.
One of the hallmark symptoms is sciatica, which is characterized by pain that radiates from the lower back down through the buttock and into the leg. This occurs when the herniated disc presses on the sciatic nerve. In addition to pain, a herniated disc can cause numbness or tingling sensations in the extremities, such as the arms or legs, due to nerve compression. Muscle weakness is another common symptom, potentially affecting coordination and the ability to perform everyday tasks. Recognizing these symptoms early can lead to a more accurate diagnosis and effective treatment plan.
diagnostic processes for herniated discs
When suspecting a herniated disc, healthcare professionals employ various diagnostic methods to confirm the condition. The process typically begins with a thorough physical examination, where a doctor evaluates reflexes, muscle strength, and the range of motion in the affected areas. This initial assessment helps identify any neurological deficits or muscle weakness that may suggest a herniated disc.
Imaging tests are vital for a definitive diagnosis. X-rays, although not capable of showing herniated discs directly, can help rule out other causes of back pain, such as fractures or tumors. MRI scans are the most effective imaging tool, providing detailed images of the spine's soft tissues, including the intervertebral discs. CT scans and myelograms may also be used to visualize the spine and detect any abnormalities. These tests collectively aid in confirming the presence and extent of a herniated disc, guiding appropriate treatment options.
self-assessment guide for herniated disc symptoms
While professional diagnosis is essential, individuals can perform a preliminary self-assessment to evaluate their symptoms. Keeping a symptom diary is a practical approach, allowing you to track pain patterns, intensity, and any potential triggers. Documenting these details can provide valuable insights during consultations with healthcare providers.
Simple physical tests at home can also help gauge flexibility and strength. For instance, gently bending forward or backward and noting any pain or discomfort can indicate areas of concern. However, it is crucial to approach these self-assessments with caution and not to rely solely on them for diagnosis. Consulting a healthcare professional is imperative to ensure an accurate diagnosis and to develop an effective treatment plan tailored to your specific needs.
Understanding the symptoms and diagnostic processes associated with herniated discs empowers individuals to take proactive steps in managing their back pain. Early recognition and intervention can significantly improve quality of life, reduce pain, and prevent further complications, underscoring the importance of being informed about this common spinal condition.
Emotional and psychological aspects of dealing with a herniated disc
Living with a herniated disc can be an emotionally challenging experience. Chronic pain often affects not only physical health but also mental well-being. Feelings of frustration, anxiety, and even depression are common as individuals navigate the limitations imposed by their condition. Acknowledging these emotional challenges is crucial for comprehensive care and recovery.
Coping mechanisms such as mindfulness, meditation, and cognitive-behavioral therapy can be beneficial in managing the psychological impact of chronic pain. Support groups, whether in-person or online, offer a platform for sharing experiences and gaining encouragement from others facing similar challenges. These resources can provide much-needed emotional support and practical advice, helping individuals maintain a positive outlook despite their condition.
Managing daily activities with a herniated disc
Adapting daily activities is essential for individuals with a herniated disc to prevent further injury and manage symptoms effectively. Ergonomic adjustments at work and home, such as using supportive chairs and maintaining proper posture, can significantly reduce strain on the spine. It is also important to avoid lifting heavy objects and to use proper techniques when bending or reaching.
Incorporating recommended exercises and stretches into your routine can help alleviate symptoms and improve mobility. Low-impact activities like swimming, walking, and yoga are excellent choices to maintain physical fitness without exacerbating pain. A balanced lifestyle that includes regular exercise, a healthy diet, and adequate rest is crucial in managing a herniated disc and promoting overall well-being.
Frequently Asked Questions
What is the difference between a herniated disc and a bulging disc?
A herniated disc occurs when the soft inner core of the disc protrudes through its outer layer, often causing nerve irritation. In contrast, a bulging disc involves the disc protruding outward without breaking through the outer layer. While both conditions can cause similar symptoms, a herniated disc is typically more severe and more likely to cause significant pain and nerve issues.
Can a herniated disc heal on its own?
Yes, a herniated disc can heal over time, especially with appropriate conservative treatments such as rest, physical therapy, and medication. Factors influencing recovery include the severity of the herniation, the individual's overall health, and adherence to treatment recommendations. In some cases, surgical intervention may be necessary if conservative measures are ineffective.
What are the treatment options for a herniated disc?
Treatment options for a herniated disc range from conservative methods to surgical procedures. Conservative treatments include physical therapy, pain medications, and lifestyle modifications. In cases where these methods do not provide relief, surgical options such as discectomy or spinal fusion may be considered to alleviate symptoms and restore function.
How can I prevent a herniated disc?
Preventing a herniated disc involves maintaining a healthy lifestyle and practicing good body mechanics. Regular exercise strengthens the muscles supporting the spine, while maintaining a healthy weight reduces strain on the back. Ergonomic practices, such as using proper posture and lifting techniques, are also essential in minimizing the risk of disc herniation.
When should I see a doctor for back pain?
It is advisable to seek medical attention if back pain persists for more than a few weeks, is severe, or is accompanied by symptoms such as numbness, tingling, or weakness in the limbs. Immediate medical care is necessary if back pain follows a traumatic injury or is associated with loss of bladder or bowel control, as these may indicate a more serious condition requiring prompt intervention.