Lower back pain is a common ailment, and herniated discs are often a significant contributor. It's estimated that up to 80% of adults experience lower back pain at some point in their lives, with herniated discs being a frequent culprit. This condition can severely impact daily activities, causing pain, reducing mobility, and diminishing overall quality of life.
understanding herniated discs in the lower back
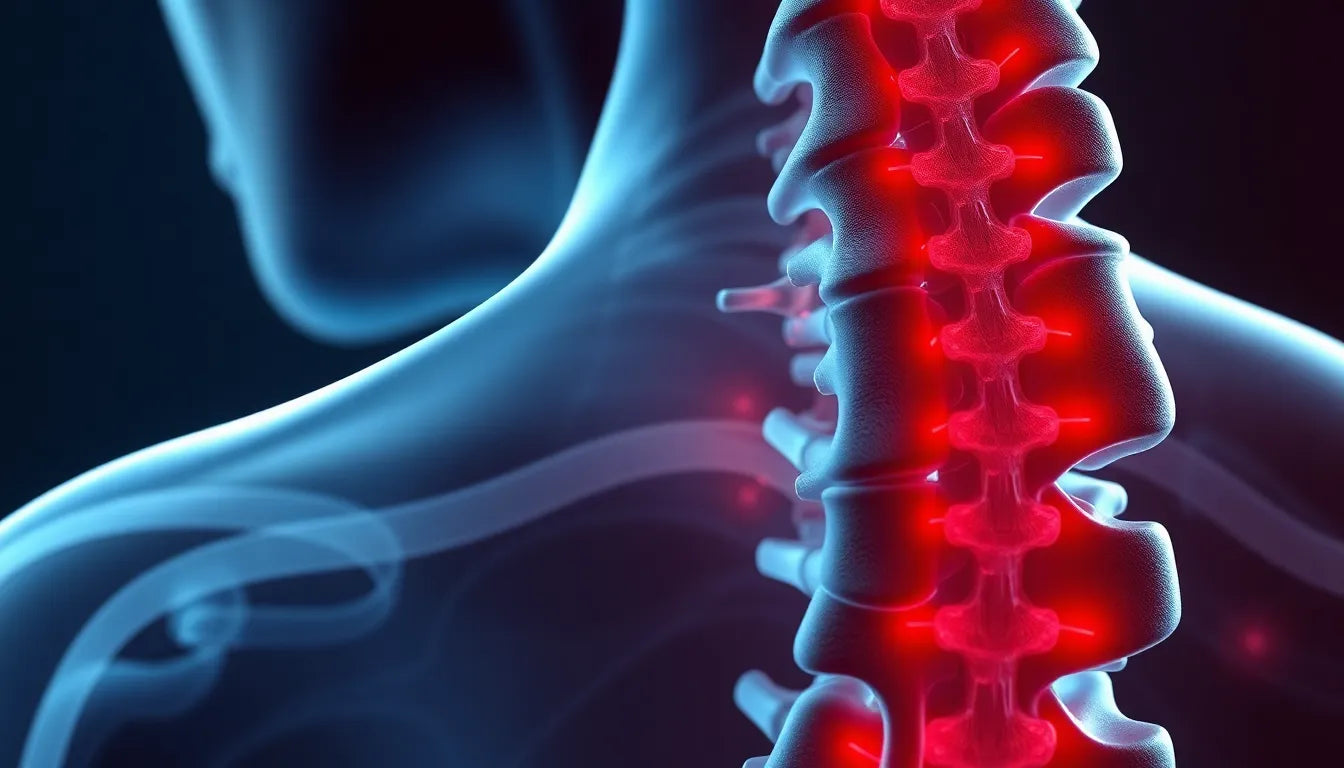
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a crack in its tougher exterior. This can happen in any part of the spine, but it's most common in the lower back, known as the lumbar region. The pressure from the herniated material can irritate nearby nerves, leading to pain, numbness, or weakness, often radiating down the legs. These symptoms can vary in intensity, from mild discomfort to severe, debilitating pain.
purpose of this post
The purpose of this blog post is to provide comprehensive information on the treatment options available for a herniated disc in the lower back. Whether you are considering nonsurgical methods like physical therapy and medications or exploring surgical interventions, it's crucial to understand the choices available. The treatment plan should be tailored to the individual's specific symptoms, severity of the condition, and personal health needs. By exploring these options, you can make informed decisions about managing your condition and improving your quality of life.
nonsurgical treatment options for herniated discs
When dealing with a herniated disc in the lower back, nonsurgical treatments are often the first line of defense. These methods aim to relieve pain and improve function without the need for invasive procedures.
rest and activity modification
Initially, rest is crucial to prevent further aggravation of the herniated disc. Avoiding activities that exacerbate symptoms, such as heavy lifting or prolonged sitting, can significantly reduce pain. Emphasizing proper body mechanics and posture during daily activities can also aid in recovery. For instance, maintaining a neutral spine position and using ergonomic furniture can help alleviate stress on the lumbar region.
medications for pain relief
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce inflammation and alleviate pain associated with a herniated disc. These medications can provide significant relief, but they are not without limitations. Long-term use may lead to gastrointestinal issues or kidney problems. Muscle relaxants may also be prescribed to ease muscle spasms, providing additional comfort. However, it's essential to use these medications under the guidance of a healthcare professional to minimize potential side effects.
physical therapy and targeted exercises
Physical therapy plays a pivotal role in treating herniated discs. A tailored exercise program can strengthen the muscles supporting the spine, improve flexibility, and reduce pain. Commonly recommended exercises include:
- Pelvic tilts: Help stabilize the lower back by strengthening the abdominal muscles.
- Knee-to-chest stretches: Alleviate tension in the lower back.
- Hamstring stretches: Improve flexibility and reduce strain on the lower back.
- Core stabilization exercises: Enhance overall spinal support.
These exercises, often guided by a physical therapist, can be instrumental in managing symptoms and preventing future episodes.
advanced nonsurgical options
For individuals who do not respond to initial treatments, advanced nonsurgical options are available. Epidural steroid injections can be administered to reduce inflammation and provide pain relief. These injections deliver corticosteroids directly to the affected area, offering temporary relief for several weeks or months.
Additionally, applying ice or heat can provide immediate, albeit temporary, relief. Ice packs can reduce swelling, while heat therapy can relax tense muscles and improve blood flow to the affected area. These simple remedies can be used in conjunction with other treatments to enhance comfort and mobility.
surgical treatment considerations
While nonsurgical methods are effective for many, surgery may be necessary for those with severe symptoms or neurological deficits. Conditions warranting surgical intervention include persistent pain that disrupts daily life or significant weakness in the legs.
types of surgical procedures
Several surgical options are available, each with its own benefits and risks. The most common procedures include:
- Microdiscectomy: This minimally invasive procedure removes the herniated portion of the disc, relieving pressure on the nerves. Recovery time is typically short, with many patients resuming normal activities within a few weeks.
- Endoscopic discectomy: Similar to microdiscectomy, this procedure uses an endoscope to remove disc material, resulting in less tissue damage and quicker recovery.
The choice of surgery depends on the patient's specific condition, overall health, and the surgeon's expertise. A detailed discussion with a healthcare provider can help determine the most appropriate course of action.
Understanding the range of treatment options for a herniated disc in the lower back is crucial for making informed decisions. Whether opting for nonsurgical methods or considering surgery, each approach should be tailored to the individual's needs, ensuring the best possible outcome.
Alternative and Complementary Therapies
In addition to traditional treatments, some individuals explore alternative therapies for managing a herniated disc in the lower back. Acupuncture, for example, involves the insertion of thin needles into specific points on the body to relieve pain and improve function. Some patients report positive outcomes, though scientific evidence remains mixed.
Chiropractic care is another option, focusing on spinal manipulation to improve alignment and reduce discomfort. While some find relief through chiropractic adjustments, it's essential to consult with a healthcare provider to determine if this approach is suitable for your condition.
Preventive Measures for Spinal Health
Preventing a herniated disc can be as important as treating one. Adopting healthy lifestyle habits can significantly reduce the risk of disc injury. Maintaining a healthy weight is crucial, as excess weight places additional stress on the spinal discs. Regular exercise, including core-strengthening activities, helps support the spine and improve flexibility.
Ergonomic aids, such as supportive chairs and adjustable desks, can also play a role in preventing disc issues. Ensuring proper posture, particularly during long periods of sitting or standing, can alleviate pressure on the lower back. Simple adjustments, like using a lumbar support cushion or positioning computer screens at eye level, can make a significant difference in spinal health.
Conclusion
Understanding and addressing a herniated disc in the lower back involves exploring a range of treatment options, from nonsurgical methods like physical therapy and medications to surgical interventions when necessary. Alternative therapies and preventive measures also offer additional avenues for managing and preventing disc problems. Consulting with healthcare professionals is essential to develop a personalized treatment plan that best fits your needs and lifestyle.
Frequently Asked Questions
What is the fastest way to heal a herniated disc in the lower back?
The fastest way to heal a herniated disc involves a combination of rest, physical therapy, and possibly medications. Avoiding activities that worsen symptoms and engaging in exercises to strengthen the back can promote recovery. In some cases, interventions like epidural steroid injections may provide quicker relief.
Can a herniated disc heal on its own?
Yes, many herniated discs can heal on their own over time with conservative treatment. The body can reabsorb the herniated material, reducing pressure on the nerves. However, this process can take weeks to months, and supportive care is often necessary to manage symptoms during this period.
How long does recovery take after surgery for a herniated disc?
Recovery time after surgery for a herniated disc varies depending on the procedure and individual factors. Generally, patients may return to normal activities within a few weeks following a microdiscectomy. Full recovery can take several months, with physical therapy often recommended to aid rehabilitation.
Are there any long-term effects of a herniated disc in the lower back?
While many individuals recover fully, some may experience long-term effects such as chronic pain or reduced mobility. Ongoing management, including exercise and lifestyle modifications, is crucial to minimize these effects and maintain spinal health.