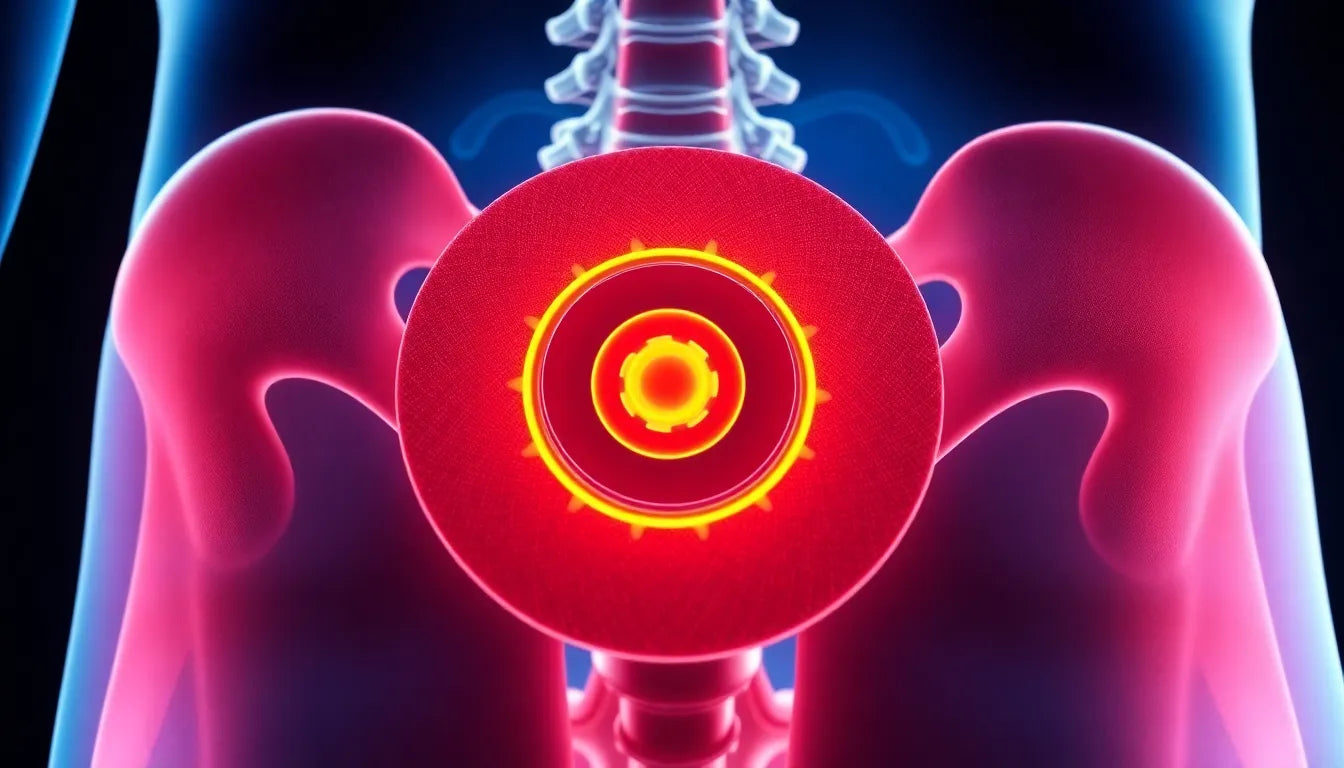
Understanding whether you have a herniated disc can be crucial for managing back pain effectively. A herniated disc, also known as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through a tear in its tougher outer layer. This condition can lead to discomfort and other symptoms, primarily because the herniated material may press on nearby nerves.
Herniated discs are a common concern, especially among individuals experiencing persistent back pain. They play a vital role in the spine by acting as cushions between the vertebrae, allowing flexibility and movement while absorbing shocks. However, when these discs herniate, they can cause significant pain and mobility issues. Understanding the prevalence of this condition is important, as it affects a significant portion of the population, particularly those aged 30 to 50. Early identification of symptoms can prevent further complications and improve treatment outcomes.
Common concerns and questions
If you're wondering, "How do I know if I have a herniated disc?" you're not alone. This is a primary concern for many experiencing back pain, as distinguishing between different spinal issues can be challenging. This blog post aims to address this question by exploring the symptoms, diagnostic methods, and key differences from other spinal conditions. By understanding these aspects, you can gain a clearer picture of your condition and take appropriate steps towards diagnosis and treatment.
This guide will provide you with essential information to help you identify if a herniated disc might be causing your pain. We'll delve into the symptoms you should look out for, the diagnostic tools used by healthcare professionals, and how herniated discs differ from other common spinal issues. Stay informed and proactive about your health by recognizing the signs early and seeking medical advice when necessary.
Symptoms of a herniated disc
Recognizing the symptoms of a herniated disc is crucial for early diagnosis and treatment. While back pain is a common symptom, it is not the only indicator. Understanding the range of symptoms can help differentiate a herniated disc from other spinal issues.
General symptoms
One of the most common symptoms of a herniated disc is pain that radiates into the arms or legs, depending on the location of the herniation. This pain is often described as sharp or burning and can be exacerbated by certain movements or positions. Additionally, individuals may experience numbness or tingling in the affected areas, which occurs when the herniated disc presses on nearby nerves.
Muscle weakness is another symptom that can significantly impact daily activities. This weakness may result in difficulty lifting or holding items, and in severe cases, it can affect one's ability to walk or maintain balance. These symptoms highlight the importance of seeking medical evaluation if a herniated disc is suspected.
Location-specific symptoms
The location of the herniated disc in the spine can influence the symptoms experienced. In the lumbar spine, or lower back, a herniated disc often causes pain in the lower back, buttocks, thighs, and calves. This is because the lumbar spine supports much of the body's weight and is involved in many movements.
In contrast, a herniated disc in the cervical spine, located in the neck, may cause pain in the neck, shoulders, and arms. This pain can be accompanied by headaches and difficulty with neck movement. Understanding these location-specific symptoms can assist in identifying the potential presence of a herniated disc.
Comparison with other conditions
It's important to differentiate a herniated disc from other spinal conditions, such as a bulging disc. While both conditions involve the discs between the vertebrae, a herniated disc is generally more severe. In a bulging disc, the disc protrudes out of its normal space but does not rupture. Symptoms of a bulging disc can be similar but are often less intense than those of a herniated disc.
Understanding these differences can aid in discussions with healthcare providers and ensure accurate diagnosis and treatment plans.
Diagnosis of a herniated disc
Accurate diagnosis of a herniated disc involves a combination of physical examinations and advanced imaging techniques. This process is essential for developing an effective treatment strategy.
Initial assessment
The diagnostic process typically begins with an initial assessment by a healthcare professional. This includes a physical examination focusing on nerve function and muscular strength. During this assessment, doctors may test reflexes, muscle strength, and the ability to feel light touches or pinpricks on the skin.
Discussion of medical history and symptom onset is also crucial. Patients should provide detailed information about when symptoms began, their severity, and how they affect daily life. This information can help guide further diagnostic testing.
Advanced diagnostic tools
For a more definitive diagnosis, advanced imaging tools are often used. MRI scans are considered the gold standard for identifying herniated discs, as they provide detailed images of soft tissues, including discs and nerves. An MRI can clearly show the location and extent of a herniation.
In some cases, additional tests such as X-rays, CT scans, or myelograms may be used. X-rays can check for bone abnormalities, while CT scans offer cross-sectional images that provide more detail than standard X-rays. Myelograms, which involve injecting dye into the spinal canal, can also help visualize the spinal cord and nerve roots.
Table: diagnostic tests and their functions
| Test Type | Purpose | Advantages |
|---|---|---|
| MRI Scan | Detailed images of soft tissues | Non-invasive, detailed |
| X-ray | Checks for bone abnormalities | Quick, widely available |
| CT Scan | Cross-sectional images | More detailed than X-rays |
By understanding the symptoms and diagnostic processes associated with herniated discs, individuals can take informed steps toward managing their condition. Early diagnosis is key to preventing further complications and improving treatment outcomes.
Treatment options and management
Once a herniated disc is diagnosed, exploring treatment options becomes crucial. Management strategies can vary based on the severity of symptoms and the individual's overall health, but they generally fall into two categories: conservative treatments and surgical interventions.
Conservative treatments
For many individuals, conservative treatments can effectively manage the symptoms of a herniated disc. These may include rest, physical therapy, and pain management techniques such as nonsteroidal anti-inflammatory drugs (NSAIDs). Physical therapy focuses on exercises that strengthen the muscles supporting the spine, improving flexibility and reducing pressure on the affected disc.
Additionally, attention to posture and the use of ergonomic aids in daily life can significantly alleviate discomfort. Making small adjustments, such as using a supportive chair or maintaining proper alignment while sitting and standing, can prevent further strain on the spine.
Surgical interventions
Surgery is typically considered when conservative treatments fail to provide relief, or if the herniated disc causes significant neurological deficits. Surgical options may include discectomy, where the herniated portion of the disc is removed, or spinal fusion, which stabilizes the spine by joining two or more vertebrae.
While surgical interventions can offer significant relief, they also carry risks such as infection or nerve damage. Therefore, a thorough discussion with a healthcare provider is essential to weigh the benefits and risks before proceeding with surgery.
Preventive measures
Preventing a herniated disc or reducing the risk of recurrence involves making lifestyle changes and adopting healthy habits. Regular exercise, particularly activities that strengthen the core muscles, can support the spine and reduce the likelihood of disc herniation.
Maintaining a healthy weight is also crucial, as excess body weight can place additional stress on the spine. Ergonomic adjustments at home and work, such as using a standing desk or adjusting the height of a computer screen, can further protect the back from strain.
Frequently asked questions
What are the early signs of a herniated disc?
Early signs of a herniated disc can include localized pain in the back or neck, radiating pain into the arms or legs, numbness, tingling, and muscle weakness. These symptoms often occur after certain activities or movements and may vary depending on the disc's location.
How long does it take to recover from a herniated disc?
Recovery time can vary widely depending on the severity of the herniation and the treatment approach. Many individuals experience relief from symptoms within a few weeks to a few months with conservative treatment. However, recovery may take longer if surgery is required.
Can a herniated disc heal on its own?
Yes, in some cases, a herniated disc can heal on its own over time as the body reabsorbs the herniated material. However, if symptoms persist or worsen, it is important to seek medical advice to prevent further complications.
What activities should be avoided with a herniated disc?
Activities that involve heavy lifting, twisting, or high-impact movements should generally be avoided to prevent exacerbating symptoms. It is advisable to consult a healthcare provider or physical therapist for personalized guidance on safe activities.
How is a herniated disc different from a bulging disc?
A herniated disc involves a rupture in the outer layer of the disc, allowing the inner material to protrude and potentially press on nearby nerves. In contrast, a bulging disc occurs when the disc protrudes out of its normal space without rupturing. Symptoms of a bulging disc are often less severe but can still cause discomfort.
By understanding treatment options, preventive measures, and common concerns, individuals can take proactive steps toward managing a herniated disc and maintaining spinal health. Early intervention and informed decision-making are key to achieving the best possible outcomes.