A herniated disc, often referred to as a slipped or ruptured disc, is a common spinal condition that can lead to significant discomfort and mobility issues. Located between the vertebrae in the spine, discs act as cushions that absorb shock and allow for flexibility and movement. When one of these discs becomes damaged or displaced, it can press on nearby nerves, causing pain and other symptoms. Understanding what a herniated disc is and how it affects the body is crucial for maintaining spinal health and preventing further complications.
Understanding the spine's anatomy
The human spine is a complex structure composed of 33 vertebrae, interspersed with intervertebral discs that provide cushioning and support. These discs have a tough outer layer, known as the annulus fibrosus, and a soft, jelly-like center called the nucleus pulposus. This unique structure allows the spine to withstand various stresses and strains while providing the flexibility needed for movement. However, when a disc becomes herniated, the inner material can protrude through the outer layer, potentially compressing nearby nerves and leading to pain and discomfort.
The prevalence of herniated discs
Herniated discs are a common condition, affecting people of all ages, but are most prevalent in individuals between the ages of 30 and 50. As we age, the discs in our spine naturally lose some of their water content, making them less flexible and more prone to injury. This degeneration, combined with other factors such as trauma or poor posture, can lead to disc herniation. Understanding the prevalence and causes of herniated discs is essential for recognizing symptoms early and seeking appropriate treatment to maintain spinal health.
The impact on daily life and common misconceptions
Living with a herniated disc can significantly impact one's quality of life, affecting daily activities and overall mobility. The pain and discomfort associated with this condition can range from mild to severe, often making it difficult to perform routine tasks or engage in physical activities. There are also several misconceptions surrounding back pain and herniated discs, with many people believing that all back pain is indicative of a herniated disc, or that surgery is the only treatment option. However, understanding the true nature of herniated discs can help dispel these myths and encourage individuals to seek comprehensive solutions for relief.
The goal of this post is to provide a thorough understanding of herniated discs, including their causes, symptoms, and available relief options. By gaining insight into this condition, individuals can make informed decisions about their spinal health and explore effective strategies for managing and alleviating pain.
Causes of herniated discs
Understanding the underlying causes of herniated discs is essential for both prevention and management. One of the primary contributors is degenerative disc disease, a condition that often accompanies aging. As we grow older, the discs in our spine naturally lose hydration and elasticity, making them more susceptible to wear and tear. This degeneration can lead to the weakening of the disc's outer layer, increasing the risk of herniation.
Another significant cause is trauma. Sudden injuries or accidents, such as falls or car crashes, can exert excessive force on the spine, potentially causing a disc to rupture. Even seemingly minor incidents, like lifting heavy objects improperly, can lead to disc herniation if the spine is subjected to undue stress.
Additionally, lifestyle factors play a crucial role in the health of spinal discs. Obesity can increase the load on the spine, accelerating disc degeneration and increasing the likelihood of herniation. A sedentary lifestyle, characterized by prolonged periods of sitting or lack of physical activity, can also weaken the muscles supporting the spine, making discs more vulnerable to injury. Poor posture, whether while sitting, standing, or sleeping, can contribute to uneven pressure on the spine, further exacerbating the risk of herniation.
Recognizing symptoms of herniated discs
The symptoms of a herniated disc can vary widely depending on the location and severity of the herniation. One of the most common symptoms is pain, which can manifest in different areas of the body. For instance, a herniated disc in the lower back may cause pain that radiates down the legs, a condition known as sciatica. Similarly, a herniated disc in the neck can lead to pain that extends into the shoulders and arms.
In addition to pain, individuals may experience neurological symptoms such as numbness, tingling, or weakness in the limbs. These symptoms occur when the protruding disc material compresses nearby nerves, disrupting normal nerve function. In severe cases, this compression can significantly affect mobility and coordination.
The progression of herniation can be categorized into stages, ranging from mild to severe. Initially, a disc may bulge slightly without causing significant symptoms. As the condition advances, the disc may rupture, leading to more pronounced symptoms and potential complications. Recognizing the early signs of herniation is crucial for seeking timely intervention and preventing further deterioration.
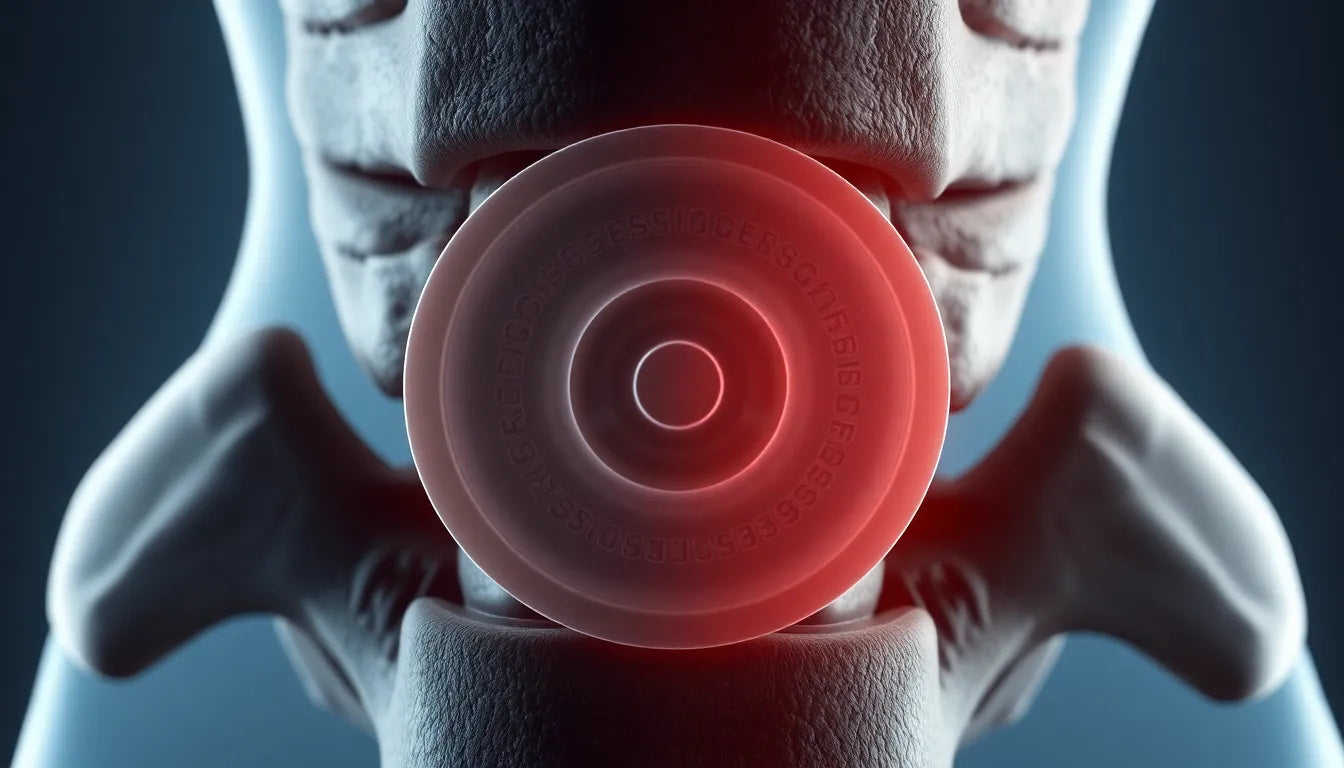
Visual aids for understanding herniated discs
To better understand the impact of herniated discs, visual aids can be incredibly helpful. A diagram of the spine highlights the location and structure of intervertebral discs, providing a clear picture of how herniation occurs. Such diagrams often illustrate the relationship between discs and surrounding nerves, helping individuals visualize the source of their symptoms.
Additionally, an infographic detailing the common symptoms and stages of herniation can serve as a quick reference for those seeking to identify and understand their condition. By combining visual elements with informative content, individuals can gain a more comprehensive understanding of herniated discs and their effects on the body.
In the next section, we will explore various treatment and relief options available for managing herniated discs, including both conservative and surgical interventions. By understanding these options, individuals can make informed decisions about their spinal health and take proactive steps toward relief and recovery.
Treatment and relief options for herniated discs
Managing herniated discs effectively requires a comprehensive approach that considers both non-surgical and surgical options. Conservative management is often the first line of treatment and includes physical therapy, medications, and lifestyle modifications. Physical therapy focuses on strengthening the muscles supporting the spine, improving flexibility, and reducing pain. Medications such as anti-inflammatories and pain relievers can help manage symptoms, while lifestyle changes, including weight management and improved posture, can prevent further injury.
In cases where conservative treatments do not provide sufficient relief, surgical interventions may be considered. Surgery is typically reserved for severe cases where the herniated disc causes significant pain or neurological symptoms that impair daily life. Common surgical procedures include discectomy, where the herniated portion of the disc is removed, and spinal fusion, which stabilizes the spine. It is essential to consult with a healthcare provider to determine the most appropriate surgical option based on individual circumstances.
Additionally, ergonomic solutions can play a crucial role in alleviating symptoms and preventing further injury. Ergonomic aids, such as supportive chairs, adjustable desks, and proper lifting techniques, can minimize strain on the spine and promote healthier posture. These solutions are particularly beneficial for individuals who spend extended periods sitting or performing repetitive tasks.
Expert insights on herniated disc management
Consulting with medical professionals, such as neurosurgeons and physical therapists, is vital for developing a personalized treatment plan for herniated discs. Dr. Emily Carter, a renowned neurosurgeon, emphasizes the importance of early intervention and tailored treatment strategies. "Each patient's condition is unique, and a personalized approach ensures the most effective management of herniated discs," she advises.
Physical therapists also play a critical role in recovery, offering exercises and techniques to strengthen the spine and improve mobility. John Davis, a certified physical therapist, highlights the significance of patient education. "Understanding the mechanics of the spine and how to protect it can empower individuals to take control of their recovery," he explains. Engaging with healthcare professionals can provide valuable insights and support throughout the treatment process.
Frequently asked questions
What is the difference between a bulging disc and a herniated disc?
A bulging disc occurs when the disc protrudes outward but remains intact, whereas a herniated disc involves a rupture of the disc's outer layer, allowing the inner material to leak out. Symptoms of a herniated disc are typically more severe due to nerve compression.
Can a herniated disc heal on its own?
In some cases, a herniated disc can heal without surgical intervention, especially with appropriate conservative treatment. Factors such as the severity of the herniation, the individual's overall health, and adherence to treatment plans influence recovery.
How long does it take to recover from a herniated disc?
Recovery time varies depending on the severity of the herniation and the treatment approach. Many individuals experience improvement within a few weeks to months with conservative management, while surgical recovery may take several months.
Are there exercises to avoid with a herniated disc?
Certain exercises, such as heavy lifting, high-impact activities, and movements that involve twisting the spine, can exacerbate symptoms. It is advisable to focus on low-impact activities like walking, swimming, and specific stretching exercises recommended by a physical therapist.
When should I see a doctor for back pain?
It is important to seek medical attention if back pain persists for more than a few weeks, is severe, or is accompanied by symptoms such as numbness, tingling, or weakness in the limbs. Early diagnosis and intervention can prevent further complications.
By understanding the available treatment options and engaging with healthcare professionals, individuals with herniated discs can take proactive steps toward managing their condition and improving their quality of life.