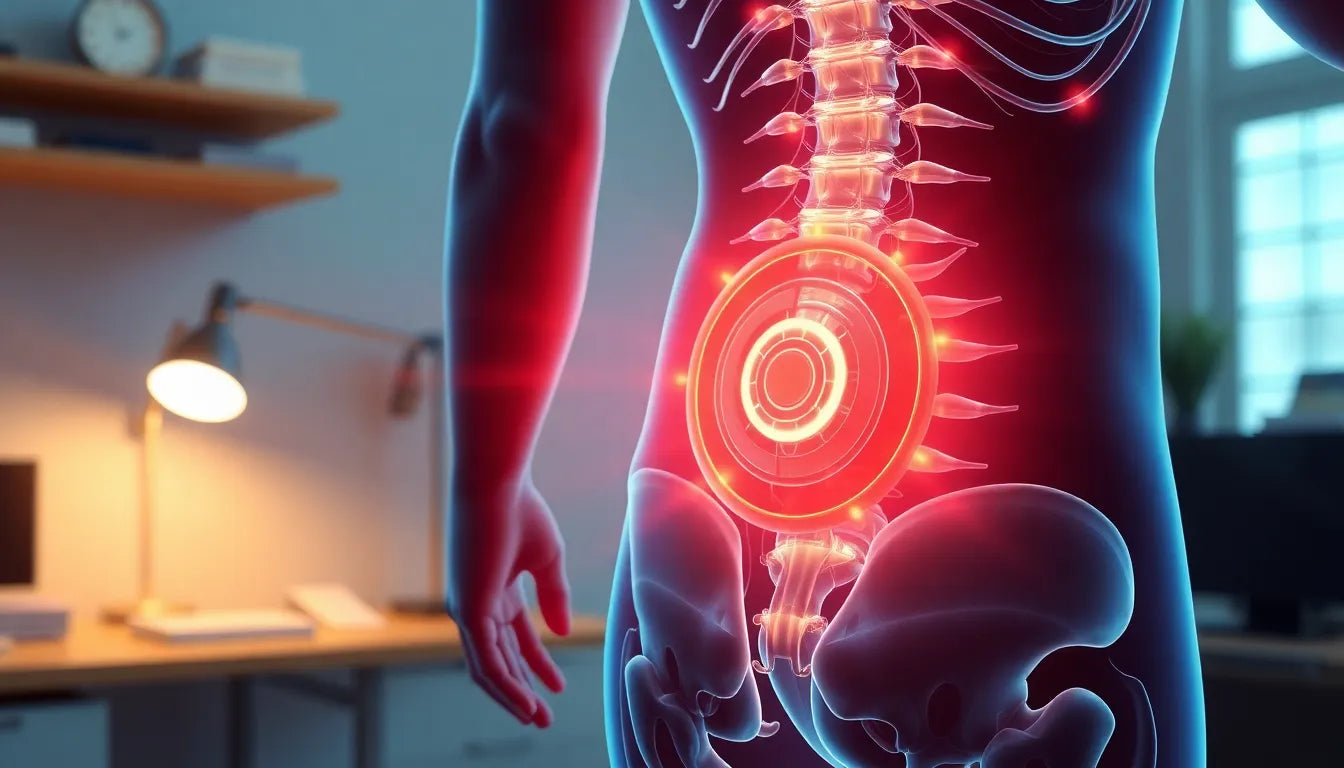
Herniated discs in the lower back, medically referred to as lumbar herniated discs, are a common spinal condition that can cause a range of symptoms. These discs act as cushions between the vertebrae, and when they become herniated, the inner gel-like core pushes through the outer layer. This can result in pain, numbness, and weakness, primarily affecting the lower extremities. The discomfort often radiates down the legs, a condition known as sciatica, which can significantly impact daily activities and quality of life.
exploring dizziness as a symptom
While dizziness is not typically associated with herniated discs in the lower back, it can occur in rare cases. This symptom may arise due to nerve compression or other related conditions that affect the body's balance and spatial orientation. When the nerves in the lumbar region are irritated or compressed, it can sometimes lead to unexpected symptoms, including dizziness, though this is more commonly linked to cervical spine issues.
purpose of this post
The aim of this post is to explore the potential link between lower back herniated discs and dizziness. Understanding these less common symptoms is crucial for a comprehensive diagnosis and effective treatment. By shedding light on the possible connections between lumbar herniated discs and dizziness, we hope to provide valuable insights for those experiencing these symptoms and seeking relief. Recognizing the full spectrum of symptoms can lead to more informed healthcare decisions and improved patient outcomes.
exploring symptoms and causes of lumbar herniated discs
In understanding the symptoms of lumbar herniated discs, it is essential to highlight the primary manifestations that patients typically experience. Common symptoms include persistent leg pain, often referred to as sciatica, which occurs when the herniated disc presses on nearby nerves. This can lead to sharp, shooting pain that travels from the lower back down to one or both legs. Additionally, patients may experience numbness and weakness in the affected leg or foot, which can impair mobility and daily functioning.
While dizziness is not a primary symptom of lumbar herniated discs, it is crucial to acknowledge the rare instances where patients report balance issues or dizziness. According to findings from Avicenna Klinik, severe nerve root irritation or spinal cord compression might lead to such secondary symptoms. This occurs because the body's response to pain and nerve disruption can sometimes affect balance and spatial orientation, although these symptoms are more frequently associated with cervical spine issues.
medical explanations for dizziness in lumbar disc herniation
The occurrence of dizziness in patients with lumbar herniated discs, although rare, can be explained through various medical perspectives. Insights from CORE Orthopedics suggest that the symptoms of a herniated disc can vary significantly depending on the location and severity of the herniation. While dizziness is not directly linked to lumbar disc issues, it may result from altered body mechanics or the stress response to chronic pain. When the body compensates for pain or discomfort, it can inadvertently affect balance, leading to sensations of dizziness.
Additionally, nerve compression in the lower back can indirectly influence other bodily functions. The autonomic nervous system, which regulates balance and coordination, might be impacted, albeit indirectly. This can sometimes result in dizziness, especially when compounded by the physical and emotional stress of dealing with chronic lower back pain.
the indirect connection between lower back issues and dizziness
Understanding the indirect causes of dizziness in the context of lumbar herniated discs is crucial for comprehensive patient care. One potential factor is the side effects of medications prescribed for pain management. Some pain relief medications can cause dizziness as a side effect, contributing to the overall sensation of imbalance experienced by the patient.
Moreover, chronic pain from a herniated disc can lead to increased stress and anxiety, which are known to exacerbate dizziness. The body's stress response can heighten sensitivity to balance disturbances, making patients more susceptible to feelings of dizziness. This highlights the importance of addressing both the physical and psychological aspects of herniated disc symptoms in treatment plans.
case studies and expert opinions
In examining the link between lower back herniated discs and dizziness, case studies and expert opinions provide valuable insights. While specific case studies focusing solely on dizziness as a symptom of lumbar herniated discs are limited, anecdotal evidence from healthcare professionals suggests that patients do occasionally report dizziness in conjunction with other symptoms.
Experts emphasize the importance of a thorough diagnostic approach to rule out other potential causes of dizziness, such as vestibular disorders or inner ear issues. By considering the full spectrum of symptoms and potential causes, healthcare providers can offer more targeted and effective treatments, improving patient outcomes.
In conclusion, while dizziness is not a common symptom of lumbar herniated discs, it is essential to recognize the potential indirect connections. By understanding the complex interplay between nerve compression, medication side effects, and stress, patients and healthcare providers can work together to address these symptoms comprehensively.
diagnosis and treatment of herniated discs and associated symptoms
Diagnosing a herniated disc in the lower back requires a comprehensive approach to accurately identify the source of symptoms and rule out other potential causes, such as vestibular disorders that could explain dizziness. Healthcare providers typically employ a combination of physical examinations, patient history, and imaging tests like MRI or CT scans to confirm the presence of a herniated disc and assess its impact on the spinal nerves.
Once diagnosed, treatment options for herniated discs focus on alleviating pain, reducing inflammation, and improving mobility. Conservative treatments often include physical therapy, which helps strengthen the muscles supporting the spine and improve posture. Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to manage pain and swelling. In more severe cases, surgical intervention might be necessary to remove or repair the herniated portion of the disc.
ergonomic solutions and lifestyle changes
Incorporating ergonomic solutions plays a significant role in managing symptoms of a herniated disc and preventing further complications. Ergonomic aids, such as supportive chairs and standing desks, help maintain proper posture and reduce strain on the lower back. Additionally, incorporating regular stretching and strengthening exercises into daily routines can alleviate tension in the spine and improve overall spinal health.
Practical lifestyle changes, like maintaining a healthy weight and avoiding prolonged sitting or heavy lifting, are also crucial in managing herniated disc symptoms. These adjustments can reduce the risk of exacerbating the condition and contribute to a more comfortable and active lifestyle.
expert insights and collaborative care
Consulting with medical professionals for personalized treatment plans is essential for effectively managing herniated disc symptoms, including any associated dizziness. Collaborating with healthcare providers, such as physical therapists and orthopedic specialists, ensures a comprehensive approach to treatment that addresses both the physical and psychological aspects of the condition.
Expert insights emphasize the importance of a multidisciplinary approach to care, which may include pain management specialists, psychologists, and nutritionists, to address the full spectrum of symptoms and improve patient outcomes. By working together, patients and healthcare providers can develop strategies that enhance quality of life and promote recovery.
frequently asked questions
Can a herniated disc in the lower back cause dizziness?
While not common, dizziness can occur indirectly through nerve compression or related conditions affecting balance.
What are the main symptoms of a herniated disc in the lower back?
Common symptoms include pain, numbness, and weakness in the legs, but dizziness is not typically a direct symptom.
How is dizziness related to spinal issues?
Dizziness may be linked to altered body mechanics or stress from chronic pain, though it is more commonly associated with cervical spine issues.
What treatments are available for managing dizziness related to herniated discs?
Treatments may include physical therapy, medication, ergonomic adjustments, and in severe cases, surgery.
How can ergonomic aids help with herniated disc symptoms?
Ergonomic aids can improve posture, reduce strain on the spine, and alleviate pain, potentially reducing dizziness.