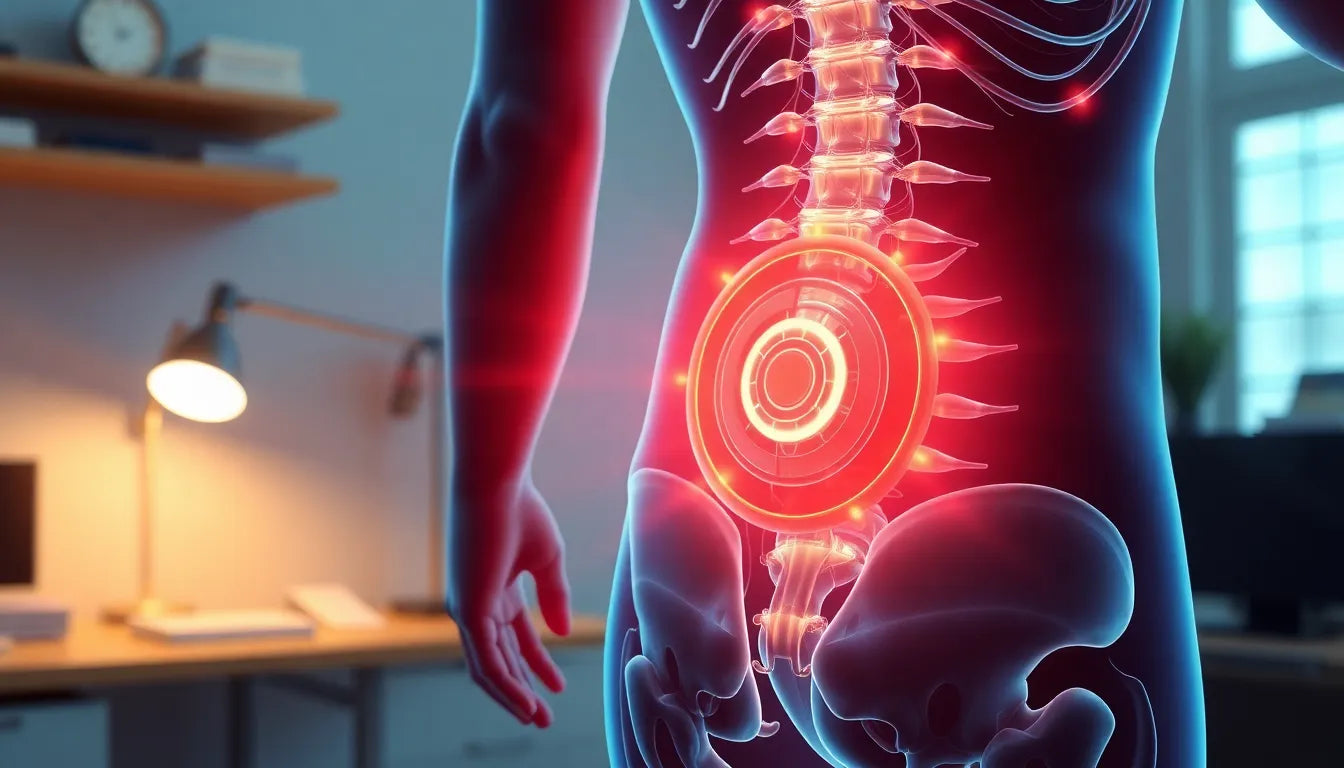
Understanding what a herniated disc means is crucial for anyone experiencing back pain or those aiming to maintain spinal health. Commonly referred to as a "slipped disc," a herniated disc occurs when the soft, jelly-like center of a spinal disc pushes through a crack in the tougher exterior casing. This condition can affect any part of the spine but is most often found in the lower back, potentially leading to pain, numbness, or weakness in an arm or leg.
the spine and intervertebral discs
The human spine is a complex structure composed of vertebrae, intervertebral discs, nerves, and muscles. The intervertebral discs act as cushions between the vertebrae, absorbing shock and allowing flexibility. These discs are made up of a tough outer layer called the annulus fibrosus and a soft center known as the nucleus pulposus. The discs play a critical role in maintaining the spine's integrity and facilitating movement.
While the spine is designed to handle a variety of movements and loads, it is not immune to wear and tear. Over time, or due to injury, the pressure on the spine can cause a disc to herniate. This condition is surprisingly common, affecting a significant portion of the population, especially those aged 30 to 50. Herniated discs can significantly impact daily life, leading to discomfort and limiting physical activity.
importance of recognizing herniated discs
Recognizing the symptoms of a herniated disc early is essential for effective management and to prevent further complications. Common symptoms include localized back pain, pain radiating down the arms or legs, numbness, and muscle weakness. Ignoring these signs can lead to chronic pain and more severe nerve damage.
Understanding what a herniated disc means and how it affects the body is the first step in addressing the issue. Early diagnosis and treatment can alleviate symptoms and improve quality of life. Untreated herniated discs can lead to persistent pain and potential long-term complications, making it imperative to seek medical advice if symptoms arise.
detailed explanation of herniated discs
A herniated disc occurs when the inner gel-like substance of the disc, known as the nucleus pulposus, protrudes through a tear or rupture in the outer layer, the annulus fibrosus. This displacement can lead to irritation or compression of nearby spinal nerves, resulting in pain and discomfort. The anatomy of the spine plays a crucial role in understanding this condition, as intervertebral discs are essential for providing flexibility and absorbing shocks that occur during daily activities.
The spine is a complex structure composed of bones (vertebrae), intervertebral discs, nerves, and muscles. The intervertebral discs act as cushions between the vertebrae, allowing for smooth movement and flexibility while absorbing impact. These discs consist of a tough outer ring, the annulus fibrosus, and a soft, jelly-like core, the nucleus pulposus. When the annulus fibrosus becomes weakened or damaged, the nucleus pulposus can push through, leading to a herniated disc.
symptoms and diagnosis
The symptoms of a herniated disc can vary depending on the location and severity of the herniation. Common symptoms include back pain, numbness, tingling, weakness, and radiating pain that can extend to the arms or legs. For instance, a herniated disc in the lower back may cause sciatica, characterized by pain that travels down the leg. Conversely, a herniated disc in the neck may lead to pain or numbness in the shoulder and arm.
Diagnosing a herniated disc typically involves a combination of physical examinations and imaging tests. Physicians may assess the patient's reflexes, muscle strength, and range of motion. Imaging techniques like MRI and CT scans are often employed to visualize the spine's condition and confirm the presence of a herniated disc.
causes and risk factors
Several factors can contribute to the development of a herniated disc. Age-related degeneration is a common cause, as the discs naturally lose hydration and elasticity over time, making them more susceptible to injury. Trauma, such as lifting heavy objects improperly or experiencing a fall, can also lead to disc herniation. Additionally, genetic predisposition and connective tissue disorders may increase the risk.
Other risk factors include occupations that involve repetitive lifting, twisting, or bending, as well as a sedentary lifestyle and poor posture. Individuals between the ages of 30 and 50 are more likely to experience a herniated disc due to these contributing factors.
types and stages of herniation
Disc herniations can be classified into different types and stages based on the extent of the nucleus pulposus displacement. The initial stage, known as disc protrusion, involves a slight bulge of the disc without a rupture. As the condition progresses, the disc may reach the extrusion stage, where the nucleus pulposus pushes through the annulus fibrosus but remains connected. In the final stage, sequestration, the nucleus pulposus breaks free and enters the spinal canal.
Understanding these stages is crucial for determining the appropriate treatment approach and predicting the potential for natural healing.
management and treatment options
Managing a herniated disc often begins with conservative treatments aimed at reducing pain and inflammation. Physical therapy is a cornerstone of non-surgical management, focusing on exercises that strengthen the core, improve flexibility, and promote proper posture. Pain management may include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants.
Lifestyle modifications, such as maintaining a healthy weight, avoiding activities that exacerbate symptoms, and incorporating ergonomic aids, can also play a significant role in managing a herniated disc. Surgery is usually considered a last resort when conservative treatments fail to provide relief. Surgical options may include discectomy, laminectomy, or spinal fusion, depending on the severity and location of the herniation.
| Treatment Option | Goals | Potential Outcomes |
|---|---|---|
| Physical Therapy | Strengthen muscles, improve flexibility, reduce pain | Improved mobility, reduced pain |
| Pain Management | Alleviate pain and inflammation | Reduced pain, increased comfort |
| Lifestyle Modifications | Prevent exacerbation, promote healing | Improved quality of life, reduced symptoms |
| Surgical Interventions | Remove disc material, relieve nerve pressure | Potential for significant pain relief, improved function |
Preventive measures for spinal health
Maintaining spinal health is crucial in preventing herniated discs and managing existing conditions. Core strengthening exercises, such as planks and pelvic tilts, are essential for supporting the spine and reducing the likelihood of disc herniation. Practicing good posture, whether sitting, standing, or lifting, can also significantly decrease spinal strain. Ergonomic aids, like supportive chairs and adjustable desks, are invaluable in promoting a healthy spine, particularly for individuals with sedentary jobs.
Incorporating these preventive measures into daily routines can help mitigate the risk of developing a herniated disc and alleviate symptoms for those already affected. It is important to tailor these practices to individual needs and consult healthcare professionals for personalized advice.
Addressing common misconceptions
There are several misconceptions about herniated discs that can lead to confusion and mismanagement. One common myth is the term "slipped disc," which inaccurately suggests that the disc has moved out of place. In reality, a herniated disc involves the nucleus pulposus pushing through a tear in the annulus fibrosus.
Another prevalent misconception is that surgery is inevitable for those with herniated discs. While surgical intervention may be necessary for severe cases, most individuals can manage their condition with conservative treatments like physical therapy and lifestyle modifications. Understanding these misconceptions can help individuals make informed decisions about their spinal health.
Case studies and personal stories
Personal stories and case studies provide valuable insights into managing herniated discs through lifestyle changes and ergonomic aids. For instance, Jane, a 45-year-old office worker, successfully alleviated her symptoms by incorporating daily core exercises and using an ergonomic chair at her desk. Her experience highlights the importance of a personalized approach to treatment and the positive impact of preventive measures.
Similarly, Mike, a construction worker, reduced his back pain by adopting proper lifting techniques and wearing supportive footwear. These anecdotes underscore the significance of adapting one's lifestyle to manage and prevent herniated disc symptoms effectively.
Visual aids for better understanding
Visual aids, such as diagrams and illustrations, can enhance comprehension of herniated discs and their treatment. Diagrams depicting the anatomy of a herniated disc can help readers visualize the condition and its impact on the spine. Additionally, videos demonstrating exercises and ergonomic adjustments can provide practical guidance for those seeking to prevent or manage herniated disc symptoms.
Incorporating these visual elements into educational resources can make complex medical concepts more accessible and engaging for a broader audience.
Frequently Asked Questions
What is a herniated disc, and how does it differ from a bulging disc?
A herniated disc occurs when the nucleus pulposus protrudes through a tear in the annulus fibrosus. A bulging disc, on the other hand, involves the disc protruding outward without a rupture. The extent of displacement is greater in a herniated disc, often leading to more severe symptoms.
Can a herniated disc heal on its own?
Yes, a herniated disc can heal naturally over time. Factors influencing recovery include the severity of the herniation, the individual's overall health, and adherence to recommended treatments. Conservative measures like physical therapy can aid in the healing process.
What activities should be avoided with a herniated disc?
Activities that place excessive strain on the spine, such as heavy lifting, twisting motions, and high-impact sports, should be avoided. Instead, individuals can focus on low-impact exercises like walking or swimming, which promote spinal health without exacerbating symptoms.
How long does it take to recover from a herniated disc?
Recovery time varies depending on the severity of the herniation and the treatment approach. Many people experience improvement within a few weeks to a few months with conservative management. However, some cases may require longer recovery periods.
Are there any long-term complications associated with herniated discs?
While many individuals recover fully, some may experience chronic pain or nerve damage if the condition is not managed properly. Ongoing management and preventive measures are crucial in minimizing the risk of long-term complications.