The unpredictability of herniated disc pain can be a source of significant frustration and confusion for those who suffer from it. One moment, life feels normal, and the next, a sudden jolt of pain can disrupt the simplest of activities. This variability in pain patterns is not only perplexing but also distressing, leaving many to wonder why herniated disc pain comes and goes.
understanding herniated disc pain
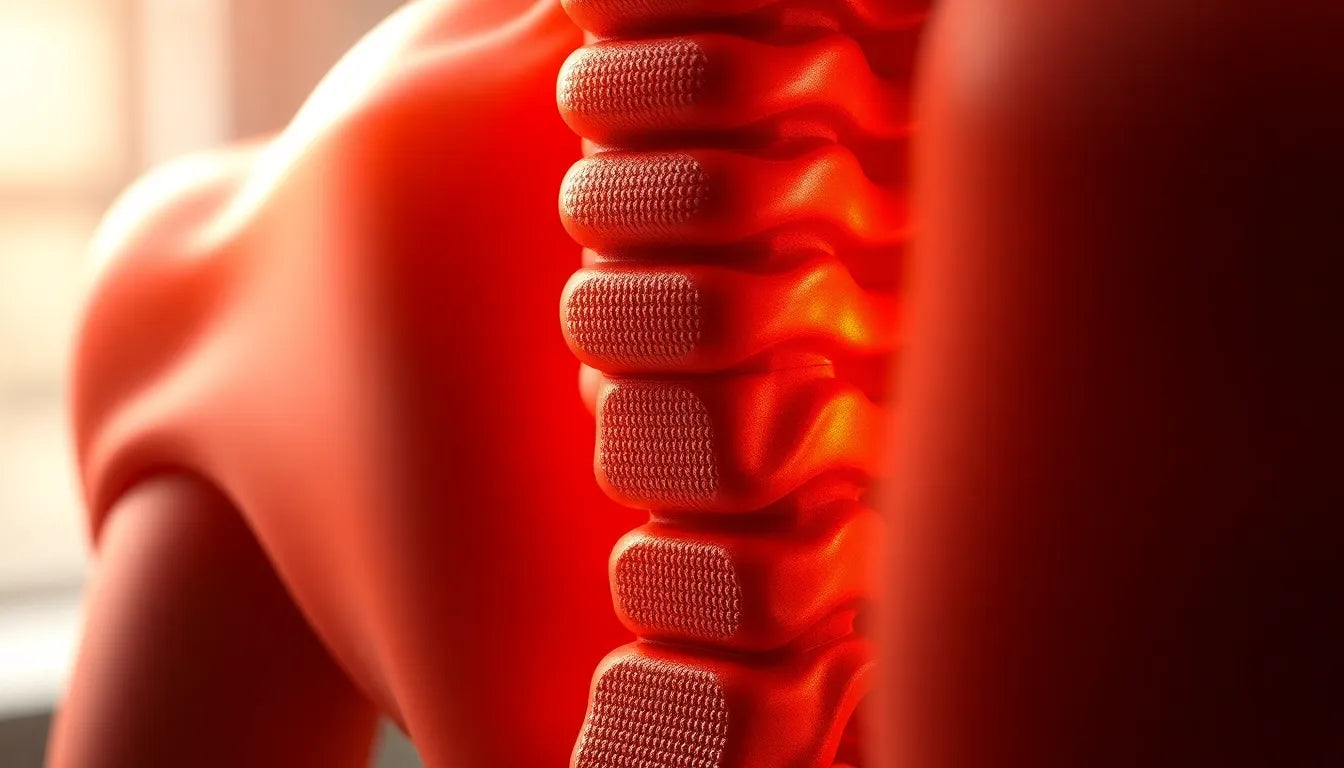
A herniated disc occurs when the soft inner gel of a spinal disc pushes through a tear in its tougher exterior. This condition can lead to nerve irritation, which is often the root cause of the pain experienced. The pain can manifest in various ways, ranging from a constant, dull ache to sharp, intermittent bursts. This inconsistency creates a mysterious and often challenging scenario for both patients and healthcare providers.
the importance of understanding pain fluctuations
Grasping the reasons behind these pain fluctuations is crucial for effective symptom management. By understanding the factors that contribute to this variability, individuals can better navigate their daily activities and make informed decisions about their treatment options. This blog will delve into the main themes that influence pain patterns, such as activity levels, posture, the natural healing process, and individual variability.
Activities like bending, lifting, or even prolonged sitting can significantly alter the intensity of herniated disc pain. Similarly, the position of the spine and the pressure exerted on the herniated disc can either exacerbate or alleviate symptoms. Moreover, the natural healing process plays a role in the fluctuation of pain, as inflammation and nerve irritation change over time.
Furthermore, each person's experience with herniated disc pain is unique. Factors such as the severity of the disc displacement and the specific nerves involved can lead to different pain patterns. Understanding these nuances is key to managing the condition effectively and improving one's quality of life.
activity and movement: key triggers in herniated disc pain
The intensity of herniated disc pain can be significantly influenced by physical activities and movements. Activities such as bending, lifting, or even prolonged sitting are known to alter the severity of pain. These movements can stretch or compress the nerves surrounding the herniated disc, leading to increased discomfort. For instance, bending forward might exacerbate the pain by placing additional pressure on the affected area, while gentle stretching or walking may help alleviate symptoms by promoting better blood flow and reducing nerve compression.
position-dependent symptoms and their impact
Another critical factor in the fluctuation of herniated disc pain is the position of the spine. Different positions can either aggravate or relieve symptoms. Sitting for extended periods often increases pressure on the lower back, potentially worsening pain. In contrast, lying down can provide relief by reducing spinal pressure. Each person's experience can vary, with some finding comfort in specific postures, such as reclining with support, while others might benefit from standing or walking.
the role of natural healing in pain fluctuations
The natural healing process also plays a significant role in the waxing and waning of herniated disc pain. As the body gradually reduces inflammation and nerve irritation, the pattern of symptoms may change. Initially, pain might be more constant, but as healing progresses, individuals may experience more intermittent pain. This fluctuation is often a positive sign, indicating that the body is responding to the injury and working towards recovery. However, patience and careful management are crucial during this period to avoid exacerbating the condition.
severity and location: how they influence pain patterns
The extent of the disc displacement and the specific nerves involved are critical in determining the nature of the pain experienced. Severe compression of a nerve can lead to continuous pain, while milder or shifting compression may result in intermittent symptoms. Additionally, the location of the herniated disc within the spine can influence which areas of the body are affected, with lumbar herniations often impacting the legs and cervical herniations affecting the arms.
chemical and mechanical irritation: a dual influence
The variability in herniated disc pain is also influenced by both mechanical pressure and chemical irritation. Mechanical pressure occurs when the protruding disc material physically compresses nerves, while chemical irritation arises from inflammatory substances released by the injured disc. These factors can lead to fluctuating symptoms, with pain levels changing based on activity, inflammation, and the body's healing response. Understanding this dual influence is essential for managing pain effectively and tailoring treatment strategies to individual needs.
In conclusion, the reasons why herniated disc pain comes and goes are multifaceted, involving a combination of physical activity, posture, natural healing, and the specific characteristics of the disc herniation. By recognizing these factors, individuals can better manage their symptoms, adjust their activities, and work towards improving their quality of life. In the next section, we will explore practical tips for managing herniated disc pain and provide answers to common questions about this condition.
Tracking pain patterns for better management
Understanding and managing herniated disc pain fluctuations is a journey that benefits significantly from personal insights. One effective method is keeping a pain diary. By documenting daily activities, pain intensity, and any associated triggers, individuals can identify patterns that may not be immediately obvious. This practice helps tailor treatment plans to individual needs, allowing for more effective management of symptoms. Recognizing specific activities or postures that exacerbate or alleviate pain can empower individuals to make informed adjustments in their daily routines.
Practical tips for managing herniated disc pain
Incorporating practical strategies into daily life can significantly improve the management of herniated disc pain. Modifying activities is essential; for instance, avoiding heavy lifting and practicing proper body mechanics can minimize strain on the spine. Adjusting posture, particularly during prolonged sitting or standing, can also alleviate discomfort. Ergonomic aids, such as lumbar support cushions or adjustable chairs, can further enhance comfort and reduce pressure on the spine. Additionally, engaging in low-impact exercises like walking or swimming can promote healing and improve overall spinal health. However, it is crucial to listen to your body and seek medical advice if pain persists or intensifies.
Frequently asked questions
What causes herniated disc pain to fluctuate?
Pain fluctuations are often due to changes in activity, posture, and the natural healing process. Movements that compress or stretch nerves can provoke symptoms, while rest or neutral positions may offer relief.
How can I manage intermittent herniated disc pain?
Managing intermittent pain involves tracking pain patterns, modifying activities, and using ergonomic aids to reduce strain. Identifying specific triggers can help tailor a personalized approach to symptom management.
When should I see a doctor about herniated disc pain?
It is advisable to seek medical attention if the pain is severe, persistent, or accompanied by other symptoms such as numbness, weakness, or loss of bladder or bowel control. Early intervention can prevent further complications.
Can herniated discs heal on their own?
Many herniated discs improve naturally over time with conservative management, such as physical therapy, rest, and lifestyle modifications. However, the healing process can vary depending on the severity and location of the herniation.
What role does inflammation play in herniated disc pain?
Inflammation can increase nerve irritation, affecting pain intensity and frequency. Reducing inflammation through lifestyle changes, medication, or therapy can help alleviate symptoms and promote healing.
By understanding the factors that influence herniated disc pain, individuals can better manage their symptoms and improve their quality of life. Adopting a proactive approach that includes tracking pain patterns and making necessary lifestyle adjustments can lead to more effective pain management and a smoother path to recovery.
Sources
- Mayo Clinic. "Herniated disk: Symptoms and causes."
- Cleveland Clinic. "Herniated Disk (Slipped or Bulging Disk)."
- Cleveland Clinic. "Why Does My Herniated Disk Pain Come & Go?"
- Woodbury Spine. "Why Does My Herniated Disk Pain Come and Go?"
- Discseel. "Herniated Disc S1-S2: Symptoms and Treatment."
- University of Maryland Medical Center. "A Patient's Guide to Lumbar Herniated Disc."