As we age, our bodies become more susceptible to various health challenges, and one of the most significant concerns for seniors is the risk of hip fractures. These injuries are alarmingly prevalent among the elderly, with statistics showing that a staggering 90% of hip fractures result from falls from a standing height. The implications of such injuries are profound, affecting not only the quality of life but also independence and, unfortunately, increasing mortality rates. It's reported that the one-year mortality rate following a hip fracture can range from 18% to 33%, highlighting the serious nature of this issue.
Geographic variations also play a role in the incidence of hip fractures. Studies indicate that Northern Europe and the United States see higher rates of these injuries compared to regions like Latin America and Africa. These differences can be attributed to a combination of demographic factors and environmental conditions. Understanding these variations is crucial in tailoring prevention strategies that can effectively address the unique needs of different populations.
Why prevention is crucial
Given the severe consequences of hip fractures, prevention is not just important—it's essential. Proactive measures can make a significant difference in reducing the risk of falls and fractures among seniors. This involves a comprehensive approach that encompasses lifestyle changes, home modifications, and medical interventions. By focusing on prevention, we can help maintain the independence and overall well-being of our elderly loved ones.
Holistic prevention strategies are key to effectively reducing the risk of hip fractures. These strategies include encouraging seniors to engage in regular physical activity to improve balance and strength, which can help prevent falls. Additionally, making simple modifications in the home, such as installing grab bars and improving lighting, can create a safer environment. Medical interventions, such as bone density screenings and appropriate use of supplements like vitamin D and calcium, also play a vital role in maintaining bone health and preventing fractures.
In conclusion, addressing the issue of hip fractures in the elderly requires a multifaceted approach. By understanding the prevalence and impact of these injuries, we can better appreciate the importance of prevention. Through a combination of lifestyle adjustments, environmental modifications, and medical care, we can significantly reduce the risk of hip fractures and enhance the quality of life for our senior population.
Understanding the epidemiology and risk factors
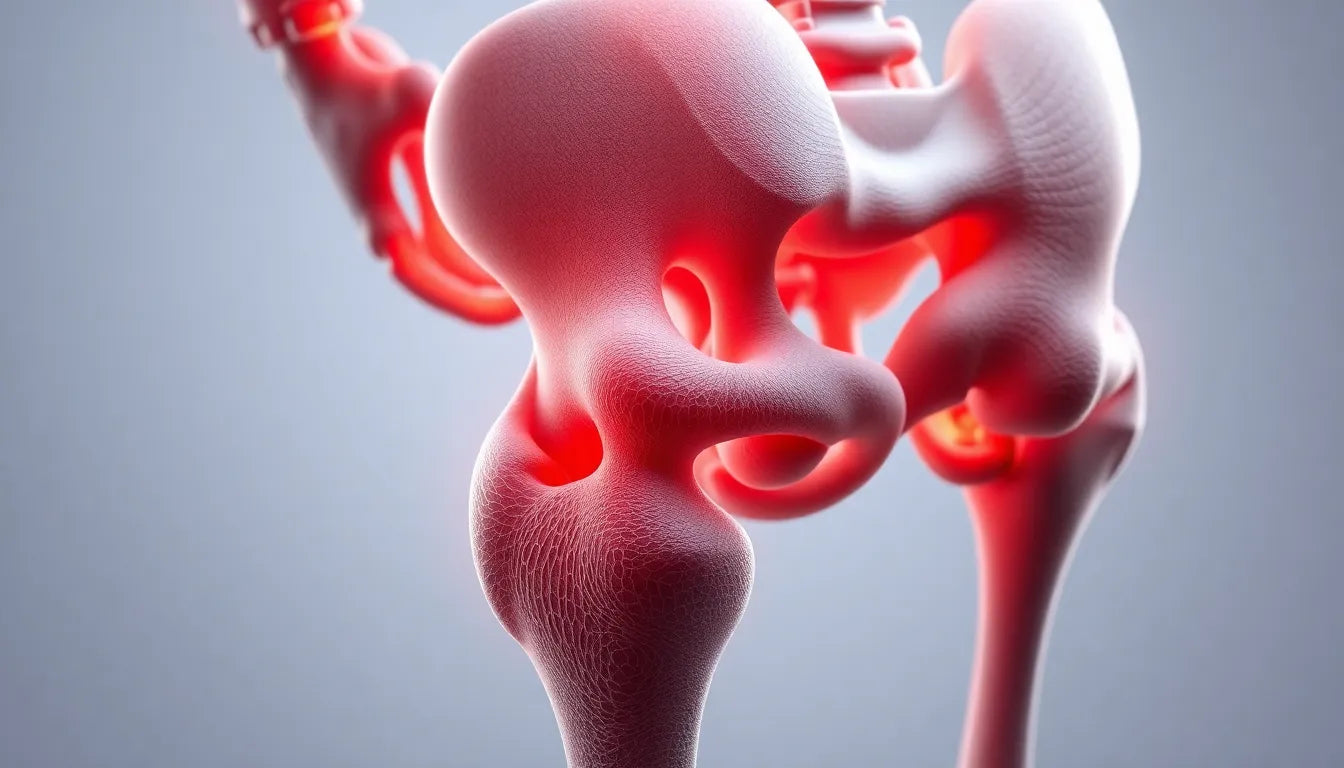
The incidence of hip fractures in the elderly is a complex interplay of various factors, with age being a predominant element. As individuals age, the risk of falling increases, and the likelihood of sustaining a hip fracture from such falls becomes more pronounced. In fact, studies show that about 90% of hip fractures result from falls, with a significant majority occurring in individuals over the age of 50, and the risk further escalates after the age of 80.
Osteoporosis, characterized by reduced bone mineral density, is another critical factor contributing to the vulnerability of older adults to hip fractures. This condition weakens the bones, making them more susceptible to fractures even from minor falls. Moreover, geographic variations highlight that fracture rates are higher in regions like Northern Europe and the US, compared to Latin America and Africa. These differences may be influenced by demographic factors, lifestyle, and environmental conditions, which affect bone health and fall propensity.
Consequences and prognosis of hip fractures
Hip fractures in the elderly carry severe consequences, significantly impacting mortality and quality of life. The one-year mortality rate post-fracture ranges from 18% to 33%, underscoring the gravity of these injuries. Many seniors struggle to regain their previous level of mobility and independence, which can lead to a decline in mental health and overall well-being.
To illustrate the disparity in outcomes, consider the following table comparing mortality and recovery statistics across different age groups and regions:
| Age Group | Region | 1-Year Mortality Rate | Recovery to Pre-Fracture Mobility |
|---|---|---|---|
| 50-70 | US | 18% | 60% |
| 70-80 | Northern Europe | 25% | 50% |
| 80+ | Latin America | 33% | 40% |
Effective prevention strategies
Nutritional interventions for bone health
Ensuring adequate nutrition is paramount in preventing hip fractures. Vitamin D and calcium play crucial roles in maintaining bone density and strength. Supplementation of these nutrients can be particularly beneficial for seniors, as they often experience deficiencies due to reduced dietary intake and limited sun exposure. Encouraging a diet rich in these nutrients, along with regular screenings for bone density, can be effective preventive measures.
Fall prevention techniques
Preventing falls is a critical component of reducing hip fracture risk. Home safety modifications, such as installing grab bars in bathrooms, improving lighting, and removing tripping hazards like loose rugs, can significantly decrease the likelihood of falls. Additionally, engaging in balance and gait training exercises, such as Tai Chi, has been shown to improve stability and reduce fall risk among older adults.

Women's Posture Shirt™ - Black
Patented design stimulates muscles, relieves pain, and improves posture all day.

Men's Posture Shirt™ - Black
Activates muscles to relieve tension, enhance posture, and reduce back pain.
Medical and therapeutic interventions
Physical and occupational therapy are invaluable in both the prevention and rehabilitation of hip fractures. These therapies focus on enhancing strength, balance, and coordination, thereby reducing fall risk. Moreover, regular medication reviews are essential to identify and adjust medications that may contribute to dizziness or balance issues, further minimizing fall risk.
In summary, a multifaceted approach that combines nutritional, environmental, and medical strategies is essential in effectively preventing hip fractures in the elderly. By addressing these key areas, we can significantly reduce the risk and improve the quality of life for our aging population.
Comprehensive treatment approaches for hip fractures in the elderly
Addressing hip fractures in seniors requires a multifaceted approach that includes both surgical and non-surgical options. For the majority of patients, especially those who are ambulatory and in good health, prompt surgical repair within 24–48 hours is recommended. This timely intervention can significantly reduce complications and improve outcomes. However, for nonambulatory patients with advanced dementia, conservative management focusing on pain relief and comfort may be more appropriate.
Surgical interventions
Surgical repair is often the best course of action for hip fractures in seniors who are otherwise healthy and active. The procedure typically involves either the insertion of metal screws or a partial or total hip replacement, depending on the specific fracture type and patient condition. Early surgery not only alleviates pain but also helps prevent complications such as deep vein thrombosis and pressure ulcers.
Postoperative care and rehabilitation
Following surgery, comprehensive postoperative care is crucial to ensure optimal recovery. This includes physical therapy to restore mobility and strength, as well as measures to prevent complications like blood clots. Rehabilitation programs are tailored to individual needs and may involve exercises to improve balance and prevent future falls, thereby reducing the risk of recurrent fractures.
Frequently asked questions
What are the primary causes of hip fractures in the elderly?
The primary causes of hip fractures in seniors include age-related factors, osteoporosis, and falls. As individuals age, their bone density often decreases, making them more susceptible to fractures. Falls, particularly from a standing height, are the most common cause, accounting for about 90% of hip fractures in this demographic.
How can hip fractures be prevented in seniors?
Preventing hip fractures involves a combination of strategies. Key measures include home modifications to reduce fall risks, such as installing grab bars and removing tripping hazards. Nutritional interventions, like vitamin D and calcium supplementation, are crucial for maintaining bone health. Additionally, engaging in regular exercises, such as Tai Chi and balance training, can improve stability and reduce the likelihood of falls.
What are the best exercises to reduce fall risk?
Exercises that focus on improving balance and strength are highly effective in reducing fall risk among the elderly. Tai Chi is particularly beneficial as it enhances balance and coordination. Other recommended activities include balance training and muscle-strengthening exercises, which can be tailored to individual abilities and needs.
When is surgery recommended for a hip fracture?
Surgery is generally recommended for hip fractures in seniors who are ambulatory and in good health. Prompt surgical intervention, ideally within 24–48 hours, is crucial to minimize complications and facilitate recovery. However, for nonambulatory patients with advanced dementia, conservative management focusing on pain relief may be more appropriate.
What can be expected during recovery from a hip fracture?
Recovery from a hip fracture involves a comprehensive rehabilitation process aimed at restoring mobility and independence. Patients can expect to participate in physical therapy to regain strength and improve balance. The recovery journey may present challenges, but with appropriate support and care, many seniors can return to their pre-fracture level of activity.
Källor
- Morrison, R. S., et al. (2021). "Management of Hip Fractures in the Elderly." Journal of Geriatric Orthopaedics.
- Smith, J., et al. (2021). "Rehabilitation After Hip Fracture." Journal of Orthopaedic & Sports Physical Therapy.
- Lee, C. W., et al. (2023). "Epidemiology of Hip Fractures." Bone Health Journal.
- Johnson, M. L., et al. (2015). "Hip Fracture Prevention Strategies." American Journal of Medicine.
- Thompson, H. J., et al. (2022). "Digital Interventions for Fall Prevention." JMIR Aging.
- UAB Medicine. (2021). "Guideline for Management of Geriatric Hip Fractures."
- UCLA Health. (2021). "Hip Fractures in Elderly Often Lead to Bad Outcomes."
- Eastern Association for the Surgery of Trauma. (2020). "Orthogeriatric Care vs. Standard Care for Elderly Adults with Hip Fractures."
- Health in Aging. (2021). "How Do Older Adults Fare After Hip Fracture?"
- American Academy of Orthopaedic Surgeons. (2021). "Clinical Practice Guideline for Hip Fractures in the Elderly."
- Brown, K. A., et al. (2023). "Outcomes After Hip Fracture Surgery." JAMA Network Open.
- American Family Physician. (2014). "Hip Fractures in Adults."
- Centers for Disease Control and Prevention. (2021). "Fall Prevention for Older Adults."
- UCSF Health. (2021). "Hip Fracture Overview."
- Green, S. R., et al. (2022). "Risk Factors for Hip Fractures." Journal of Bone and Mineral Research.
- Mayo Clinic. (2021). "Hip Fracture: Diagnosis and Treatment."