Degenerative changes in the lumbar spine are a common topic of concern, especially for those experiencing back discomfort or who have recently undergone imaging tests like MRIs or X-rays. Simply put, these changes refer to the wear and tear of the spine's structures, including the discs and joints, which naturally occur as we age. While the term might sound alarming, it's important to note that such changes are a natural part of the aging process and do not always result in pain or serious health issues.
Understanding lumbar spine degeneration
As we age, the components of our spine, particularly in the lumbar region, undergo changes that can be described as degenerative. These changes often include the thinning and drying out of intervertebral discs, which act as cushions between the vertebrae. Additionally, the development of bone spurs and the deterioration of the cartilage in the facet joints are common. Although these changes are widespread, they do not necessarily lead to severe pain or disability. Many individuals with degenerative changes in their lumbar spine live without any significant symptoms.
Clarifying terminology: degenerative disc disease and more
It's crucial to understand the terminology often associated with lumbar spine degeneration. Terms such as "degenerative disc disease," "lumbar spondylosis," and "arthritis" are frequently used interchangeably, though they have specific meanings. Degenerative disc disease refers to the condition where discs lose their cushioning ability, while lumbar spondylosis encompasses the overall degenerative process affecting the spine. Arthritis in this context typically refers to the wear and tear of the spinal joints. Understanding these terms can help patients better interpret medical reports and engage in informed discussions with healthcare providers.
The importance of early recognition
Recognizing the early signs of lumbar spine degeneration is crucial for effective management. Symptoms might include mild to moderate back pain, stiffness, or discomfort that worsens with activity. Early intervention often involves conservative management strategies, such as physical therapy, lifestyle modifications, and ergonomic adjustments, which can significantly improve quality of life. By addressing symptoms early, individuals can often avoid more invasive treatments and maintain an active lifestyle.
In summary, while degenerative changes in the lumbar spine are a natural part of aging, understanding them can alleviate unnecessary worry. By familiarizing yourself with the terminology and recognizing early symptoms, you can take proactive steps toward effective management and maintain a healthy, active life.
anatomy and pathophysiology of lumbar spine degeneration
To fully grasp the impact of degenerative changes in the lumbar spine, it's essential to understand the basic anatomy and function of this region. The lumbar spine consists of five vertebrae, labeled L1 to L5, which are the largest and bear the most weight. Between these vertebrae are intervertebral discs, which serve as shock absorbers, allowing flexibility and movement in the spine.
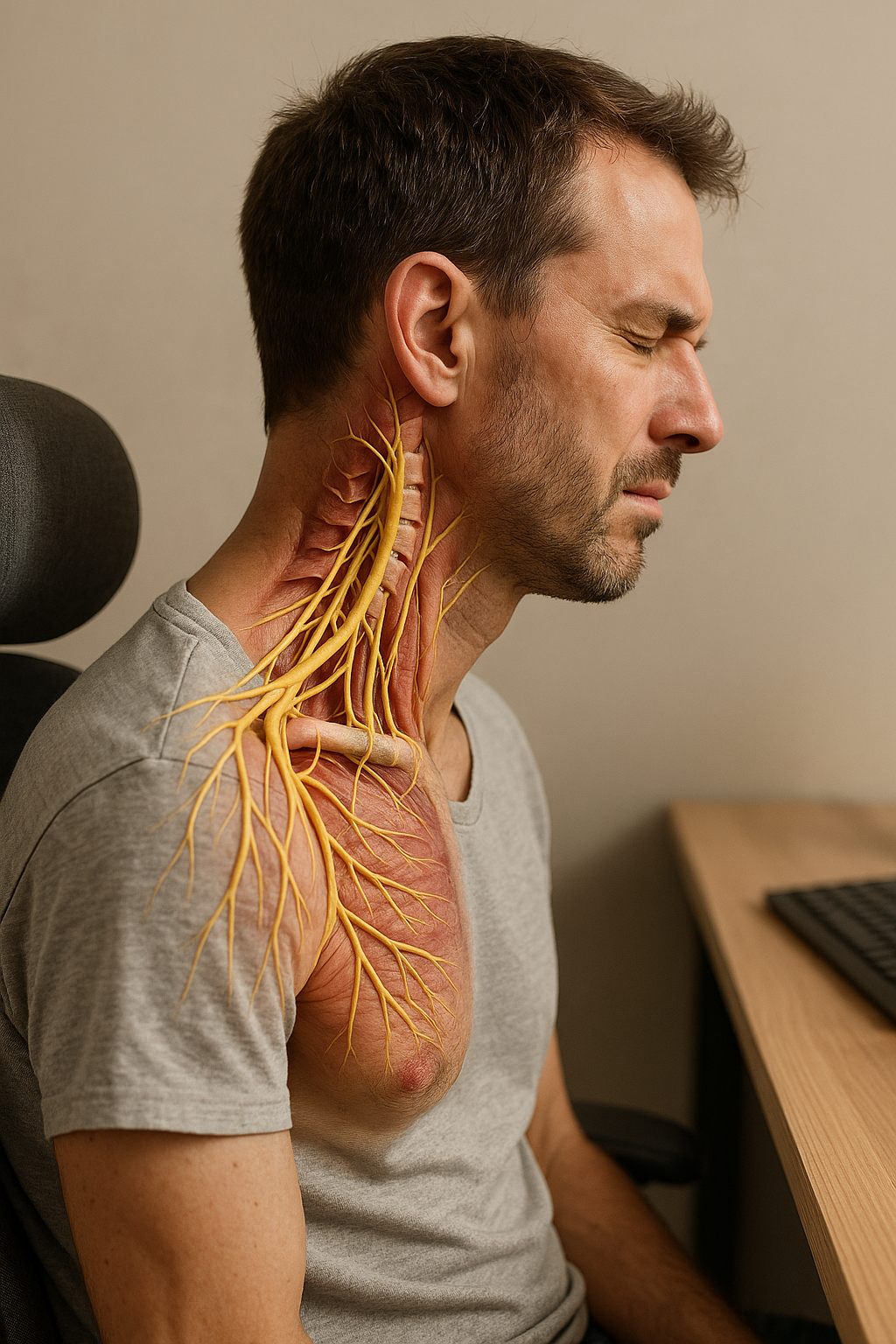
During the degeneration process, these discs undergo significant changes. They may lose hydration, leading to a decrease in disc height and elasticity. This dehydration process is a hallmark of degeneration and can result in reduced cushioning between the vertebrae, potentially leading to discomfort or pain. The most commonly affected levels are L4–L5 and L5–S1, which bear the brunt of mechanical stress.
symptoms versus imaging findings
One of the most challenging aspects of lumbar spine degeneration is the discrepancy between symptoms and imaging findings. Many individuals with significant degenerative changes on an MRI or X-ray may experience little to no pain, while others with mild changes might suffer from severe discomfort. Typical symptoms include low back pain, stiffness, sciatica, and numbness. However, it's crucial to recognize that not all abnormalities visible on imaging will correlate with pain or functional limitations.
It's important to be aware of red flags that necessitate urgent medical attention, such as changes in bowel or bladder function, severe or progressive weakness, or significant numbness. These symptoms could indicate a more serious condition, such as cauda equina syndrome, requiring immediate evaluation.
causes and risk factors of lumbar spine degeneration
Several factors contribute to the development of degenerative changes in the lumbar spine. Aging is the most significant factor, as the spine naturally undergoes wear and tear over the years. Genetics also play a role, with some individuals being predisposed to faster degeneration due to familial traits. Prior injuries to the back can accelerate the degenerative process, as can lifestyle factors like smoking and obesity, which can affect the spine's blood supply and overall health.
Poor posture and repetitive heavy lifting or bending can exacerbate degenerative changes. These activities place additional strain on the lumbar spine, potentially leading to faster wear and tear. Addressing these lifestyle factors through modifications and ergonomic adjustments can be a crucial part of managing and slowing the progression of degeneration.
diagnosis and prognosis of lumbar spine degeneration
The diagnosis of lumbar spine degeneration typically involves a combination of clinical examination and imaging tests such as MRI or X-ray. These tools help visualize the extent of degeneration and rule out other potential causes of symptoms. Common terms found in MRI reports, such as "disc desiccation," "osteophytes," and "facet joint arthrosis," describe specific degenerative changes that can be translated into layman's terms for better understanding.
While structural changes due to degeneration are often irreversible, the prognosis for symptom improvement is generally positive with appropriate management. Many individuals experience relief from symptoms through conservative treatments, and the focus is on improving function and quality of life rather than reversing the structural changes themselves.
stages of lumbar spine degeneration
The progression of lumbar spine degeneration can be categorized into stages, each characterized by specific changes and symptoms. Initially, there is a dysfunction stage where minor changes occur, often without symptoms. As degeneration progresses, discs may dehydrate and lose height, leading to increased pressure on the spine's joints and nerves.
Understanding these stages can help in anticipating potential symptoms and planning appropriate management strategies. Visual aids such as charts can be helpful in illustrating the stages and their associated symptoms, providing a clear picture of the degenerative process without causing undue alarm.
Conservative treatment and self-management
When it comes to managing degenerative changes in the lumbar spine, conservative treatment is often the first and most effective approach. Movement and physical therapy play a crucial role in maintaining flexibility and strength in the lumbar region. Regular exercise, including stretching and strengthening routines, can help alleviate pain and improve function. Additionally, pain relief options such as over-the-counter medications, heat, and ice therapy can provide temporary relief from discomfort.
Ergonomics and posture strategies are also essential components of self-management. Proper posture while sitting, standing, and lifting can significantly reduce stress on the lumbar spine. Incorporating ergonomic aids such as lumbar supports and posture shirts, like those offered by Anodyne, can enhance comfort and support during daily activities. These products are designed to promote proper alignment and reduce strain, making them a valuable part of a comprehensive management strategy.

Lumbar support belt
Provides stabilization and relief for lower back pain. Adjustable for optimal lumbar support.

Women's Posture Shirt™ - Black
Activates muscles and helps relieve pain. Improves posture for work and daily life.
Advanced treatment options
In some cases, more advanced treatments may be necessary. Injections, such as epidural steroid injections, can provide relief for individuals experiencing significant pain or nerve-related symptoms. These injections help reduce inflammation and can offer temporary relief for those who do not respond to conservative measures.
Surgery is generally considered a last resort and is reserved for cases where conservative treatments have not provided adequate relief, or when there are severe symptoms such as nerve compression. Surgical options may include procedures like discectomy or spinal fusion, depending on the specific condition and its severity. However, it's important to note that surgery comes with risks and should be carefully considered in consultation with a healthcare professional.
Living with degenerative changes
Living with degenerative changes in the lumbar spine requires a proactive approach to self-care. Long-term strategies include maintaining a healthy lifestyle with regular exercise, a balanced diet, and weight management to reduce stress on the spine. Psychological aspects, such as managing stress and anxiety related to the condition, are also important. Engaging in activities that promote relaxation and mental well-being can positively impact overall health and quality of life.
Practical tips for adapting to daily life include making ergonomic adjustments at work and home, such as using supportive chairs and desks, and pacing activities to avoid overexertion. These adaptations can help manage symptoms and maintain functionality, allowing individuals to continue with their daily routines with minimal disruption.
Frequently asked questions
What are degenerative changes in the lumbar spine?
Degenerative changes in the lumbar spine refer to the age-related wear and tear affecting the spine's discs and joints. These changes are common and often not dangerous.
Are these changes reversible?
While structural changes are not reversible, symptoms can often be managed effectively through conservative treatments and lifestyle modifications.
Can lifestyle changes impact degeneration?
Yes, maintaining a healthy weight, practicing proper posture, and engaging in regular exercise can help slow the progression of degenerative changes and reduce symptoms.
When should I see a doctor?
It is advisable to see a doctor if you experience severe pain, numbness, or changes in bowel or bladder function, as these may indicate more serious underlying issues.
How can I manage daily pain?
Daily pain can be managed through ergonomic aids, regular movement, and appropriate pain relief strategies, such as using heat or ice therapy and over-the-counter medications.
Källor
- Frontiers in Bioengineering and Biotechnology. (2024). "Degenerative Changes in the Lumbar Spine."
- Mayo Clinic Health System. "Pain Relief for Worn Spinal Disks."
- National Center for Biotechnology Information. "Degenerative Disc Disease."
- Spine-Health. "Lumbar Degenerative Disc Disease Treatment."
- National Center for Biotechnology Information. "Understanding Lumbar Spine Degeneration."
- Medical News Today. "What to Know About Degenerative Disc Disease."
- Nature. "Research on Lumbar Spine Degeneration."
- Hospital for Special Surgery. "Spondylosis and Lumbar Degeneration."
- Mayo Clinic. "Clinical Trials on Degenerative Disk Disease."
- Cleveland Clinic. "Degenerative Disk Disease Overview."
- University of Michigan Health. "Care for Degenerative Disc Disease."
- Ortho Georgia. "Lumbar Degenerative Disc Disease."
- Hospital for Special Surgery. "Degenerative Disc Disease Treatments."
- Cedars-Sinai. "Degenerative Disc Disease Information."